
ΝΙΚΟΣ ΑΝΤΩΝΙΑΔΗΣ
Χθες ήταν τα πρώτα προκαταρκτικά. Σήμερα συνεχίζουμε και η ιστορία θα πηγαίνει κλιμακωτά.
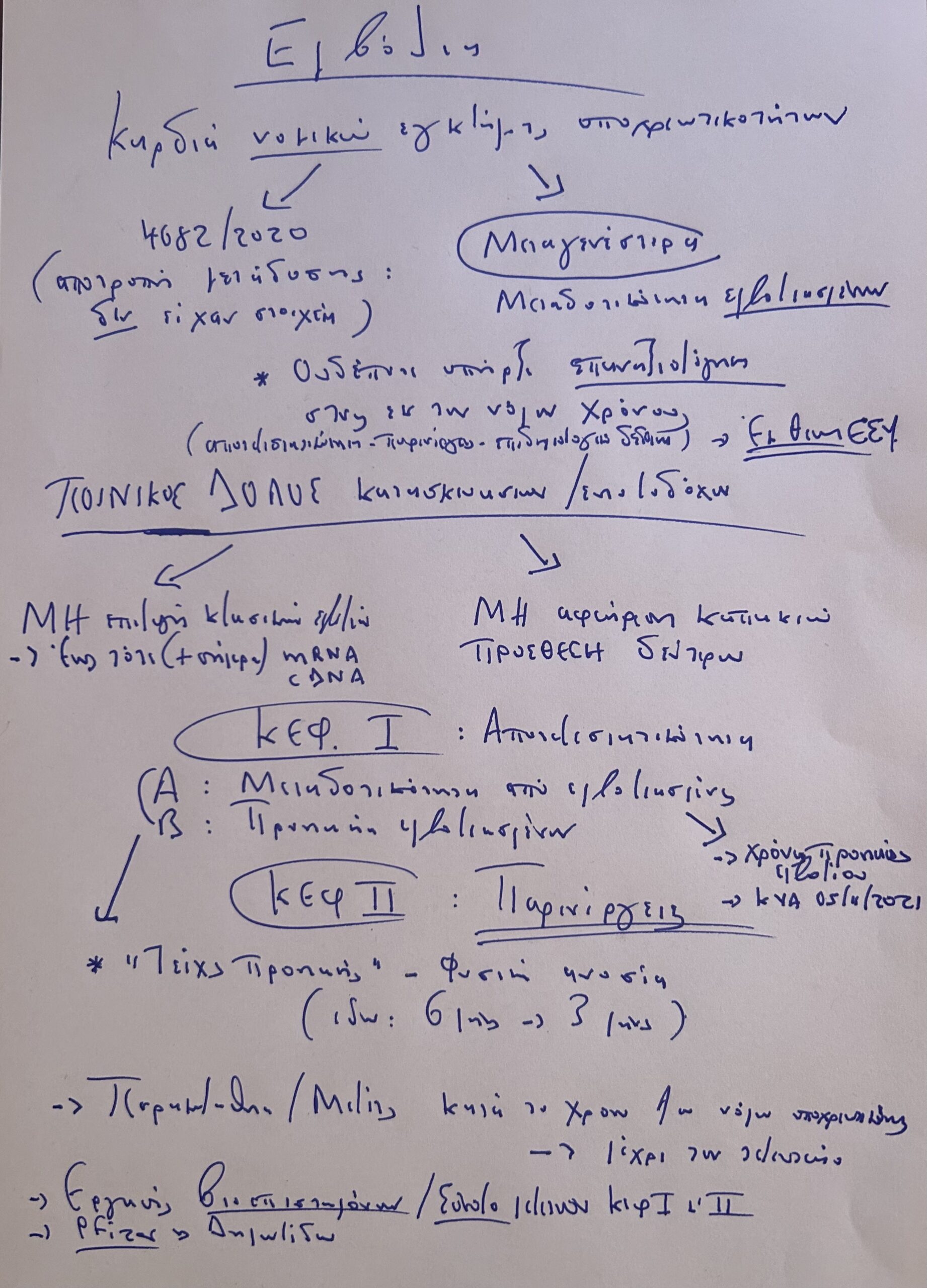
Αυτό που βλέπετε είναι ένα πρόχειρο χειρόγραφο σχέδιο της στρατηγικής της νομικής επίθεσης για τα εμβόλια:
Αυτή είναι η πρώτη σελίδα της κατατεθείσας μήνυσής μου κατά υπουργείου και ΣτΕ.:
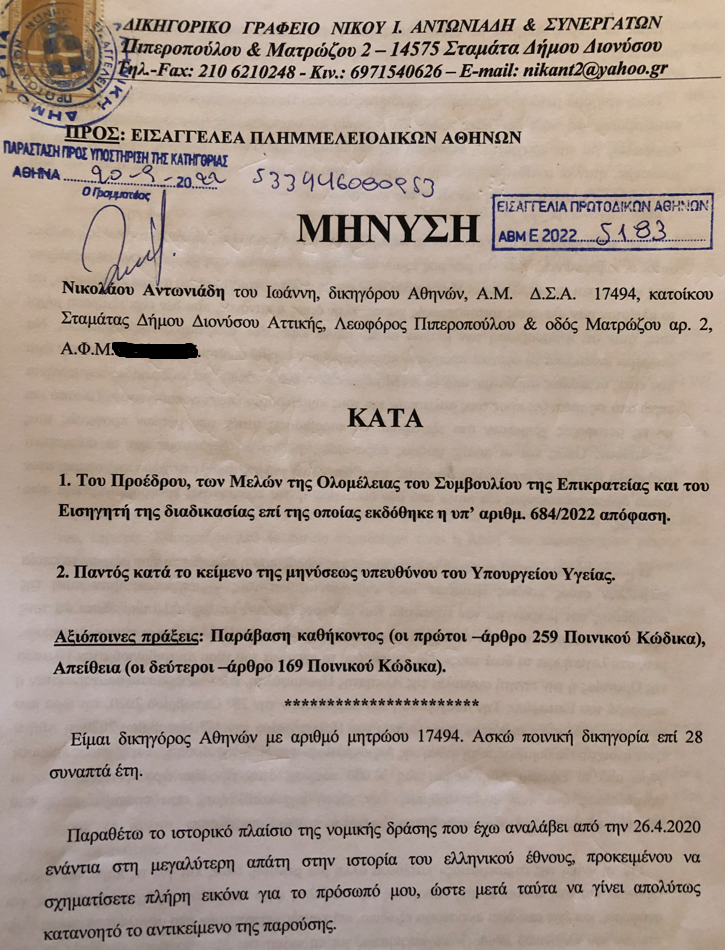
Στο κείμενο που ακολουθεί στο τέλος της εισαγωγής, θα καταλάβετε πώς κουμπώνει η μήνυσή μου της 20/09/2022 στην ποινική διαδικασία για τα εμβόλια που άρχισε να κινείται στο 6ο Προανακριτικό Τμήμα του Πταισματοδικείου Αθηνών, κατόπιν εντολής της Εισαγγελίας Πρωτοδικών Αθηνών, η οποία εκτέλεσε παραγγελία της ανώτερης εισαγγελικής αρχής της χώρας, της Εισαγγελίας Εφετών Αθηνών.

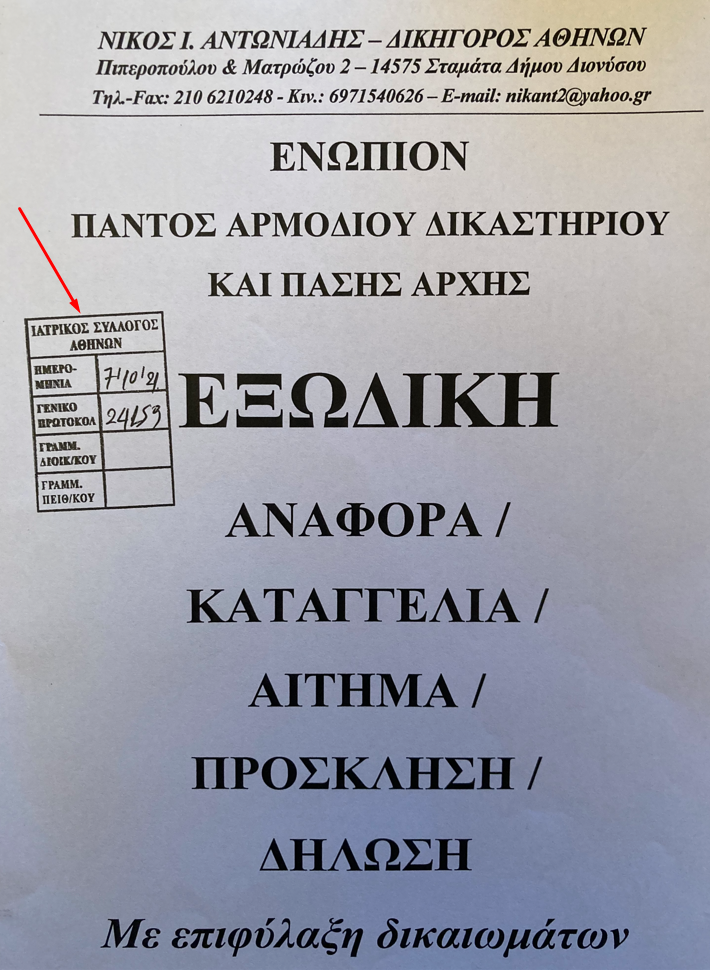
Δείτε τον τεράστιο όγκο των μελετών για τις παρενέργειες των εμβολίων που απέκρυψε η αρμόδια διεύθυνση του υπουργείου Υγείας. Αυτό που ακολουθεί στο τέλος είναι ένα …μικρό απόσπασμα από το υπόμνημα που θα καταθέσω στο 6ο Προανακριτικό Τμήμα την άλλη εβδομάδα, μαζί με τα στοιχεία των συντακτών της εξωδίκου επιστημονικής αναφοράς της 5ης Αυγούστου 2021, που ζητάει η εισαγγελική αρχή για να καταθέσουν. Η αναφορά δηλαδή που δεν απαντήθηκε ποτέ, καίτοι επιδόθηκε σε όλες τις αρμόδιες αρχές και δεν αμφισβητήθηκε ούτε μισή λέξη της.
Την είχα μάλιστα καταθέσει και στον Ιατρικό Σύλλογο Αθηνών, αλλά και εκεί η φωνή των ΠΡΑΓΜΑΤΙΚΩΝ ειδικών επιστημόνων παρέμεινε φωνή βοώντος εν τη ερήμω.
Το υπόμνημα που θα καταθέσω [για αρχή] στην ποινική διαδικασία [όπου θα πάω μαζί με τον Δημήτρη Ποντίκα, ο οποίος θα καταθέσει πρώτος από τους συντάκτες της αναφοράς (γιατί ΤΩΡΑ είναι η πραγματική ώρα του Δημήτρη)], θα συνοδεύεται από τις δύο επιστημονικές εργασίες που αποτελούν τη συνέχεια αυτής της 5ης Αυγούστου 2021, η οποία πλέον μοιάζει με …ορεκτικό μπροστά σε αυτές στο τραπέζι της κάθαρσης του εγκλήματος των εμβολίων. Μόνο η τεράστια διαφορά στον αριθμό των παραπομπών από 131 σε άνω των χιλίων, μιλάει από μόνη της.
Αλλά δεν είναι μόνο αυτό. Μου έχουν βγει τα μάτια από το διάβασμα και βουίζουν τα αυτιά μου από τις τηλεφωνικές επικοινωνίες. Είναι τρομακτικό το περιεχόμενό τους. Αυτό που κάνω εγώ, είναι, μετά την κατανόηση των επιστημονικών αναλύσεων [βλέπετε, αφού πρώτα έγινα …πνευμονολόγος, για τις ανάγκες του πρωτοκόλλου του θανάτου, έπρεπε να γίνω και …μοριακός βιολόγος, για τις ανάγκες του πρωτοκόλλου του μαζικού εμβολιασμού (ενώ για το πρωτόκολλο της απάτης, τόσο εν γένει όσο και ειδικότερα εντός ενός εκάστου των άλλων δύο, αρκούσε το λίγο μυαλό που έχω…)], είναι να μεταφράσω τα μοριακά βιολογικά σε νομικά ποινικά…
Να εντοπίσω τα στοιχεία εκείνα που τεκμηριώνουν και δένουν το δόλο των εδώ εκτελεστικών οργάνων των ξένων δολοφόνων. Και αυτά, εντοπίζονται τόσο στο πεδίο της “αποτελεσματικότητας” των εμβολίων όσο και σε αυτό -ΚΥΡΙΩΣ- των παρενεργειών τους. Σε αυτό το πεδίο, ο δόλος εντοπίζεται τόσο στη ΜΗ επιλογή των κλασικών εμβολίων όσο και, ΑΦΕΝΟΣ, σε ΑΥΤΟ που δεν αφαίρεσαν από την ουσία, ΑΦΕΤΕΡΟΥ, σε ΑΥΤΟ που ΠΡΟΣΕΘΕΣΑΝ.
Είναι τα δύο …καπάκια του στυλό, στο ΑΠΑΓΟΡΕΥΜΕΝΟ ΒΙΝΤΕΟ…



Στο σκηνικό της τεκμηρίωσης του δόλου και στα δύο πεδία, πολύ σημαντικό ρόλο έχει η υποχρεωτικότητα που επιβλήθηκε, και η οποία έχει πολλά στοιχεία από το πρωτόκολλο της απάτης εντός αυτού του μαζικού εμβολιασμού. Όπως σας είπα και στο 15λεπτο βίντεο που ανέβασα προχθές, ο νόμος 4682/2020 προέβλεψε την υποχρεωτικότητα με ΜΟΝΑΔΙΚΟ ΣΚΟΠΟ την αποτροπή της ΜΕΤΑΔΟΤΙΚΟΤΗΤΑΣ από πρόσωπα για τα οποία υπάρχουν εύλογες υπόνοιες ότι μπορούν να μεταδώσουν τη νόσο.
ΟΧΙ για να μην κολλήσουν τα ίδια και ασθενήσουν.
Οπότε, όπως είπα και στο παραπάνω βίντεο, είναι σαν να είχαν …μελέτες που να έδειχναν ότι οι πυροσβέστες μεταδίδουν τη νόσο, εν αντιθέσει π.χ. με τους αστυνομικούς, για τους οποίους, όπως άλλωστε είχε δηλώσει ο Άκης Σκέρτσος, …δεν υπήρχαν αντίστοιχες μελέτες, ώστε οι αστυνομικοί απέφυγαν την υποχρεωτικότητα. Έτσι, επιβλήθηκε μόνο στους πυροσβέστες, ώστε να αποφευχτεί η μετάδοση της νόσου στα …φλεγόμενα δάση. Τα αυτά και για τους άνω των 60, για τους οποίους προέκυψαν, ως φαίνεται, εύλογες υπόνοιες ότι με το που πατούσαν τα 60 άρχιζαν ξαφνικά να μεταδίδουν. Ενώ μία μέρα πριν …δεν μετέδιδαν.
Όσον αφορά στο μεγαλύτερο έγκλημα όλων, ως προς τις υποχρεωτικότητες, αυτό σε βάρος των υγειονομικών μας αλλά και σε βάρος της δημόσιας υγείας, με την άνευ της ελαχίστης επιστημονικής τεκμηρίωσης [η αντίθετη τεκμηρίωση υπήρχε] απομάκρυνση χιλιάδων ιατρών και νοσηλευτών από τα δημόσια νοσοκομεία της χώρας [και η δραματική αυτή έλλειψη φάνηκε πολύ γρήγορα με ολόκληρα τμήματα να μην λειτουργούν με αυταπόδεικτο τεράστιο κίνδυνο της δημόσιας υγείας], πρέπει να γίνει κατανοητό ότι θα πρέπει να ξεχάσουμε ότι μιλάμε για ιατρονοσηλευτικό (και διοικητικό) προσωπικό στα δημόσια νοσοκομεία, αλλά για απλά ανθρώπινα όντα. Θα πρέπει δηλαδή μέσα σε αυτό το σκηνικό του παραλόγου, να υπήρξαν μελέτες ή έστω με κάποιο μαγικό τρόπο “εύλογες υπόνοιες”, ότι τα συγκεκριμένα ανθρώπινα όντα, όταν αποφάσισαν να γίνουν ιατροί ή νοσηλευτές ή να δουλέψουν ως διοικητικό και άλλο προσωπικό στα δημόσια νοσοκομεία, άρχιζαν αίφνης (με το πτυχίο τους ή έστω με την απόκτηση της ειδικότητας…), να μεταδίδουν πάσης φύσεως κορωνοϊούς.
Φυσικά, το σκηνικό αυτό του παραλόγου και της απίστευτης απάτης της υποχρεωτικότητας, έχει “εξήγηση”:
Διότι” έπρεπε” να το φτάσει στα άκρα η εγκληματική οργάνωση για να πείσει τον τρομοκρατημένο πληθυσμό για την “σοβαρότητα” της κατάστασης:
“Δείτε μέχρι πού φτάσαμε, που κανονικά αυτά δεν συμβαίνουν σε δημοκρατικά καθεστώτα παρά μόνο σε φασιστικά, όπως σε αυτό του ναζισμού με τα πειράματα στα στρατόπεδα συγκεντρώσεως, αλλά …τόσο σοβαρή είναι η κατάσταση που …αναγκαστήκαμε”.
Έλα όμως που στην πραγματικότητα ΑΥΤΟ ΑΚΡΙΒΩΣ συνέβη:
Η μετατροπή δηλαδή ενός ολόκληρου πλανήτη σε ένα απέραντο Νταχάου…
Γιατί βεβαίως, τα παραπάνω περί του νόμου 4682/2020 είναι παρονυχίδα μπροστά στον ορυμαγδό των στοιχείων που σκοπίμως απεκρύβησαν από τους εγκληματίες. Ακόμα και αν δεχόμασταν ότι η κυβέρνηση δεν δρα ως εγκληματική οργάνωση, αλλά ως κανονική κυβέρνηση που θέλει το καλό των πολιτών, και υπερέβη τα προβλεπόμενα από τον νόμο 4682/2020 και έλαβε τις αποφάσεις για την υποχρεωτικότητα τόσο για την αποτροπή της μεταδοτικότητας όσο και για την αποτροπή της νόσησης, κυρίως της βαριάς, των διασωληνώσεων και των θανάτων, τα στοιχεία που αποκρύπτονταν κάθε φορά που λάμβαναν μέτρα υποχρεωτικότητας ή παρέτειναν τα μέτρα που είχαν ήδη λάβει (ΧΩΡΙΣ ΠΟΤΕ ΝΑ ΕΠΑΝΑΞΙΟΛΟΓΟΥΝ ΤΑ ΔΕΔΟΜΕΝΑ, όπως όριζαν οι σχετικές διατάξεις που ΟΙ ΙΔΙΟΙ είχαν θεσπίσει), ήταν συντριπτικά εναντίον των υποχρεωτικοτήτων, τόσο αναφορικά με τα επιδημιολογικά κάθε φορά δεδομένα όσο ως προς την “αποτελεσματικότητα” των εμβολίων, και ΚΥΡΙΩΣ ως προς τις παρενέργειες αυτών. Αποδείχθηκε κατά τη διάρκεια της ισχύος των μέτρων, ότι οι εμβολιασμένοι κολλούσαν τον ιό ΤΟΥΛΑΧΙΣΤΟΝ εξίσου με τους ανεμβολίαστους [ενώ υπάρχουν ακλόνητα στοιχεία ότι σε πάρα πολλές περιπτώσεις (ιδίως με την παραλλαγή ΔΕΛΤΑ) οι εμβολιασμένοι είχαν υψηλότερο ιικό φορτίο από τους ανεμβολίαστους], αρρώσταιναν βαριά, οδηγούντο στις Μ.Ε.Θ. και από εκεί στους τάφους.
Αλλά οι εγκληματίες άφησαν εκτός τους ανεμβολίαστους και κράτησαν εντός τους εμβολιασμένους υγειονομικούς, ΧΩΡΙΣ ΚΑΝ ΤΗΝ ΥΠΟΧΡΕΩΣΗ ΔΙΑΓΝΩΣΤΙΚΩΝ ΤΕΣΤ, με αποτέλεσμα να κολλάνε κατά κόρον οι ασθενείς σε όλη τη χώρα και ολόκληρα νοσοκομεία (θυμάστε τι έγινε π.χ. σε αυτό της Κυπαρισσίας;) να χτυπάνε κόκκινο από τους μεταδοτικούς (και πολλές φορές, με βάση και πάλι αδιαμφισβήτητες μελέτες, ΥΠΕΡΜΕΤΑΔΟΤΙΚΟΥΣ) εμβολιασμένους υγειονομικούς, τους οποίους είχαν ήδη εκθέσει στις φριχτές παρενέργειες του εμβολιασμών τους, τις οποίες ΓΝΩΡΙΖΑΝ και τις ΠΕΡΙΜΕΝΑΝ ΒΑΣΕΙ ΤΟΥ ΕΓΚΛΗΜΑΤΙΚΟΥ ΣΧΕΔΙΟΥ ΤΟΥΣ με τα συγκεκριμένα mRNA και cDNA εμβόλια.
Αλλά αυτά περί Νταχάου και αποκρύψεων, θα τα δούμε στη συνέχεια, όταν έρθει η ώρα και για τα …καπάκια, που είναι υπεύθυνα για το ασύλληπτο σακάτεμα του πληθυσμού και τους ξαφνικούς θανάτους που σαρώνουν. Και τότε θα μιλήσουμε ΚΑΙ για τους ξαφνικούς αυτούς θανάτους, με ΣΥΓΚΕΚΡΙΜΕΝΑ ΣΤΟΙΧΕΙΑ που θα προκύψουν από την εισαγγελική έρευνα με στοχευμένη έρευνα.
Διευκρινίζεται ότι στην ποινική διαδικασία ΔΕΝ υφίσταται η έννοια των προσωπικών δεδομένων…
Μέσα δε σε αυτό το σκηνικό της απάτης, έχουμε και τα επιμέρους αποδεικτικά στοιχεία. Το “τείχος ανοσίας”, η μεγάλη αυτή απάτη, η “πανδημία των ανεμβολίαστων”, μία άλλη μεγάλη απάτη, το 6μηνο της φυσικής ανοσίας [η οποία υποτιμήθηκε σκόπιμα ως ένα από τα αμέτρητα παραδείγματα της ανατροπής, στο πλαίσιο της απάτης, ιατρικών παραδοχών και δεδομένων δεκαετιών, αν όχι …αιώνων) που λίγο αργότερα έγινε 3μηνο [με τη ψυχρή ομολογία των εγκληματιών ότι μείωσαν το χρόνο για να “εκβιάσουν”], το αλαλούμ με τα “επικαιροποιημένα” εμβόλια, που άλλα έλεγε ο Πλεύρης και άλλα έλεγαν οι “ειδικοί”, για να μη ξεχνάμε και εκείνη την απίστευτη K.Y.A. της 5ης Νοεμβρίου 2021, με την οποία οι εμβολιασμένοι προ εξαμήνου πολίτες αφέθηκαν ελεύθεροι να αλωνίζουν, ενώ την ίδια ώρα από τους ίδιους “ειδικούς” που εισηγήθηκαν την Κ.Υ.Α., θεωρούντο πρακτικά ανεμβολίαστοι.
Κι όμως.
ΟΛΑ ΑΥΤΑ εδώ είναι απλά η συνέχεια των …προκαταρκτικών που άρχισαν χθες.
Το “βαρύ πυροβολικό” δεν έχει εμφανιστεί ακόμα…
*********************************************
ΙΔΟΥ [Βλ. παρακάτω] περισσότερες από 1000 ΔΗΜΟΣΙΕΥΜΕΝΕΣ μελέτες που αναφέρονται σε παρενέργειες των εμβολίων, οι οποίες προφανώς αφορούν μόνο τις βραχυπρόθεσμες παρενέργειες (καθώς δεν μπορούμε στο σημείο αυτό να έχουμε δεδομένα των μεσοπρόθεσμων και μακροπρόθεσμων παρενεργειών, παρά μόνο ενδείξεις). Υπενθυμίζουμε ότι στις 07/09/2021, 16/09/2021 και 30/09/2021, το Συμβούλιο της Επικρατείας, όπως αναφέρεται στη με αρ. 1684/2022 απόφασή του, απέστειλε προς την αρμόδια Διεύθυνση Δημόσιας Υγείας του Υπουργείου Υγείας τρία (3) υπομνηστικά έγγραφα, με τα οποία ζήτησε να γνωρίσει εγγράφως στο Δικαστήριο, μεταξύ άλλων, ποιες είναι οι τυχόν παρενέργειες από τα εμβόλια και σε τι ποσοστό ανέρχονται αυτές επί του συνόλου των εμβολιασμών, τόσο στη χώρα μας, όσο και σε ευρωπαϊκό/διεθνές επίπεδο.
ΩΣΤΟΣΟ, ουδέποτε υπήρξε απάντηση στα ερωτήματα αυτά.
Άραγε αγνοούσαν οι κρατικές αρχές όλα αυτά τα στοιχεία που ΗΤΑΝ ΚΑΤΑ ΤΕΚΜΗΡΙΟ ΓΝΩΣΤΑ ΣΕ ΑΥΤΕΣ;
-ΑΝ δεν τα αγνοούσαν, τότε ΓΙΑΤΙ ΔΕΝ ΤΑ ΠΡΟΣΚΟΜΙΣΑΝ;
-ΑΝ τα αγνοούσαν, τότε τα ΑΓΝΟΟΥΣΑΝ ΣΚΟΠΙΜΑ, καθώς ΔΕΝ ΝΟΕΙΤΑΙ σε ένα ΤΟΣΟ ΚΟΛΟΣΣΙΑΙΑΣ ΣΗΜΑΣΙΑΣ ΙΑΤΡΙΚΟ ΖΗΤΗΜΑ να μην ενδιαφέρθηκαν να τα ΑΝΑΖΗΤΗΣΟΥΝ.
-Ώστε ΠΡΟΦΑΝΩΣ και ΚΑΤΑ ΤΕΚΜΗΡΙΟ οι αρμόδιες αρχές (ΕΠΙΤΡΟΠΕΣ, «ΕΙΔΙΚΟΙ» ΕΝΤΟΣ ΚΑΙ ΕΚΤΟΣ ΕΠΙΤΡΟΠΩΝ & ΥΠΟΥΡΓΕΙΟ ΥΓΕΙΑΣ – ΚΥΒΕΡΝΗΣΗ) Δ Ε Ν ΤΑ ΑΓΝΟΟΥΣΑΝ.
Και όταν εδώ μιλάμε ΜΟΝΟ για τις ΠΑΡΕΝΕΡΓΕΙΕΣ και όχι ΚΑΙ για τον ορυμαγδό επίσης των στοιχείων για τα ΕΠΙΔΗΜΙΟΛΟΓΙΚΑ ΔΕΔΟΜΕΝΑ κατά τη διάρκεια του εμβολιαστικού προγράμματος και -ΚΥΡΙΩΣ- για τη ΜΗ ΑΠΟΤΕΛΕΣΜΑΤΙΚΟΤΗΤΑ (ΜΕΤΑΔΟΣΗ & ΠΡΟΣΤΑΣΙΑ) των εμβολίων, ο ΔΟΛΟΣ των εγχώριων ΕΚΤΕΛΕΣΤΙΚΩΝ ΟΡΓΑΝΩΝ είναι κάτι παραπάνω από ΑΠΟΔΕΔΕΙΓΜΕΝΟΣ, τόσο για τον εμβολιασμό του πληθυσμού εν γένει όσο και για τον εξαναγκασμό μερίδας αυτού να εμβολιαστεί:
ΕΙΝΑΙ ΠΡΩΤΟΦΑΝΗΣ ΚΑΙ ΤΡΟΜΑΚΤΙΚΟΣ !
ΠΛΕΟΝ, η αρμόδια Διεύθυνση Δημόσιας Υγείας του Υπουργείου Υγείας ΕΛΕΓΧΕΤΑΙ ΠΟΙΝΙΚΑ για το αδίκημα της ΑΠΕΙΘΕΙΑΣ (άρθρο 169 Ποινικού Κώδικα), για την ΑΡΝΗΣΗ να προσκομίσει στο Συμβούλιο της Επικρατείας τα ανωτέρω δεδομένα, το δε Συμβούλιο της Επικρατείας ΕΛΕΓΧΕΤΑΙ ΕΠΙΣΗΣ ΠΟΙΝΙΚΑ για το αδίκημα της παράβασης καθήκοντος (άρθρο 259 Ποινικού Κώδικα), για την παράλειψή του να ανακοινώσει στον αρμόδιο εισαγγελέα την τελεσθείσα αξιόποινη πράξη της αρμόδιας Διεύθυνσης Δημόσιας Υγείας του Υπουργείου Υγείας, ως είχε εκ του νόμου υποχρέωση (άρθρο 38 § 1 Κώδικα Ποινικής Δικονομίας). Η ποινική διαδικασία για αμφότερες κατά τα άνω πλευρές, κινήθηκε κατόπιν της υπ’ αριθμ. Α.Β.Μ. Ε22-5183 μήνυσής μου, η οποία κατατέθηκε στην Εισαγγελία Πλημμελειοδικών Αθηνών την 20/09/2022. Η δικογραφία σήμερα βρίσκεται στα χέρια του εισαγγελέα, με στοιχεία ΕΓ62-2023/110, μετά από ήδη δύο στάδια προκαταρκτικής εξέτασης, στα προανακριτικά τμήματα των Πταισματοδικείων Μαραθώνα και Αθηνών. Έχει ΠΟΛΥ ΜΕΓΑΛΟ ΕΝΔΙΑΦΕΡΟΝ να δούμε ΤΙ ΑΠΑΝΤΗΣΕ η αρμόδια Διεύθυνση Δημόσιας Υγείας του Υπουργείου Υγείας:
ΓΙΑΤΙ δεν έστειλε ΟΥΤΕ ΜΙΣΟ δεδομένο για τις παρενέργειες των εμβολίων;
Σε όλο αυτό τον κόλαφο των συντριπτικών στοιχείων, να ΜΗ ΞΕΧΝΑΜΕ ότι η υποχρεωτικότητα στις εργασιακές και πληθυσμιακές ομάδες που εφαρμόστηκε, ως ΜΟΝΑΔΙΚΟ «ΝΟΜΙΜΟ» ΣΚΟΠΟ είχε, βάσει του νόμου 4682/2020 που θέσπισε την υποχρεωτικότητα, την ΑΠΟΤΡΟΠΗ ΤΗΣ ΜΕΤΑΔΟΣΗΣ του κορωνοϊού σε τρίτους και ΟΧΙ την «προστασία» των προσώπων που υποχρεώθηκαν να εμβολιαστούν.
Διαβάζαμε π.χ. τότε για την υποχρεωτικότητα του εμβολιασμού στους άνω των 60, ότι «ο Πρωθυπουργός ανήγγειλε για πρώτη φορά την υποχρεωτικότητα στους ανεμβολίαστους άνω των 60 ετών. Στην απόφαση οδήγησε προφανώς η διαρκής αύξηση των θανάτων και των διασωληνώσεων. Και οι συνάνθρωποί μας που κατά μεγάλη πλειοψηφία πεθαίνουν ή βρίσκονται διασωληνωμένοι στις ΜΕΘ είναι 60+».
ΠΡΑΓΜΑΤΙ, στο άρθρο 24 του νόμου του νόμου 4685/2021, που έχει ως τίτλο «Υποχρεωτικότητα εμβολιασμού», διαβάζουμε ότι «για επιτακτικούς λόγους προστασίας της δημόσιας υγείας, εμβολιάζονται υποχρεωτικά κατά του κορωνοϊού COVID-19 όλα τα φυσικά πρόσωπα που έχουν την κατοικία ή τη συνήθη διαμονή τους εντός της Ελληνικής Επικράτειας και έχουν γεννηθεί έως και την 31η.12.1961».
ΠΛΗΝ ΟΜΩΣ, βάσει του νόμου 4682/2020, με τον οποίο θεσμοθετήθηκε η υποχρεωτικότητα του εμβολιασμού [κύρωσε την από 25.2.2020 Π.Ν.Π. «Κατεπείγοντα μέτρα αποφυγής και περιορισμού της διάδοσης κορωνοϊού» (Α΄ 42)], ΧΩΡΙΣ ΠΕΡΙΟΡΙΣΜΟ ως προς το εύρος της (δηλαδή με βάση τις σχετικές διατάξεις του νόμου, η κυβέρνηση έχει τη δυνατότητα να υποχρεώσει ακόμα και ολόκληρο τον πληθυσμό, «αξιολογώντας» τον «κίνδυνο»), ΡΗΤΑ προβλέπει ως ΜΟΝΑΔΙΚΟ ΣΚΟΠΟ της υποχρεωτικότητας τη ΜΗ ΜΕΤΑΔΟΣΗ του κορωνοϊού:
«Άρθρο πρώτο – Μέτρα πρόληψης, υγειονομικής παρακολούθησης και περιορισμού της διάδοσης της νόσου – Τα μέτρα αυτά συνίστανται: (α) στην ΥΠΟΧΡΕΩΤΙΚΗ ΥΠΟΒΟΛΗ ΣΕ κλινικό και εργαστηριακό ιατρικό έλεγχο, υγειονομική παρακολούθηση, ΕΜΒΟΛΙΑΣΜΟ, φαρμακευτική αγωγή και νοσηλεία ΠΡΟΣΩΠΩΝ, ΓΙΑ ΤΑ ΟΠΟΙΑ ΥΠΑΡΧΟΥΝ ΕΥΛΟΓΕΣ ΥΠΟΝΟΙΕΣ ΟΤΙ ΜΠΟΡΟΥΝ ΝΑ ΜΕΤΑΔΩΣΟΥΝ ΑΜΕΣΑ Ή ΕΜΜΕΣΑ ΤΗ ΝΟΣΟ»
Υπενθυμίζουμε ότι η κυβέρνηση της Ελλάδας ενήργησε με …πρωτοφανή αντανακλαστικά στη θέσπιση της υποχρεωτικότητας, επιδεικνύοντας …εξίσου πρωτοφανή προνοητικότητα, βλέποντας …πολύ μακριά, όταν εξέδωσε τη σχετική Πράξη Νομοθετικού Περιεχομένου την 25/02/2020 (η οποία απλά κυρώθηκε με το νόμο 4682/2020), ΠΡΙΝ ΚΑΝ, δηλαδή, κηρύξει πανδημία ο Π.Ο.Υ., την 11/03/2020.
Όλα ήταν «οργανωμένα» από την αρχή…
Ακολουθεί κατάλογος >1000 αξιολογημένων μελετών από διάφορα ιατρικά περιοδικά που αφορούν πλειάδα ανεπιθύμητων ενεργειών στους λήπτες των εμβολίων κατά της COVID-19
- Study to Describe the Safety, Tolerability, Immunogenicity, and Efficacy of RNA Vaccine Candidates Against COVID-19 in Healthy Individuals; A Study to Evaluate Safety and Immunogenicity of mRNA-1273 Vaccine to Prevent COVID-19 in Adult Organ Transplant Recipients and in Healthy Adult Participants; A Study of Ad26.COV2.S for the Prevention of SARS-CoV-2-Mediated COVID-19 in Adult Participants(ENSEMBLE) [Internet]. 2022. Available from:
https://clinicaltrials.gov/ct2/show/NCT04368728;
https://clinicaltrials.gov/ct2/show/NCT04860297;
https://clinicaltrials.gov/ct2/show/NCT04505722;
https://clinicaltrials.gov/ct2/show/NCT04470427.
ΚΑΡΔΙΑΚΕΣ ΒΛΑΒΕΣ
Μυοκαρδίτιδα
- Myocarditis after mRNA vaccination against SARS-CoV-2, a case series: https://www.sciencedirect.com/science/article/pii/S2666602221000409
- Myocarditis after immunization with COVID-19 mRNA vaccines in members of the US military. This article reports that in “23 male patients, including 22 previously healthy military members, myocarditis was identified within 4 days after receipt of the vaccine”: https://jamanetwork.com/journals/jamacardiology/fullarticle/2781601
- Association of myocarditis with the BNT162b2 messenger RNA COVID-19 vaccine in a case series of children: https://pubmed.ncbi.nlm.nih.gov/34374740/
- Acute symptomatic myocarditis in seven adolescents after Pfizer-BioNTech COVID-19 vaccination: https://pediatrics.aappublications.org/content/early/2021/06/04/peds.2021-052478
- Myocarditis and pericarditis after vaccination with COVID-19 mRNA: practical considerations for care providers: https://www.sciencedirect.com/science/article/pii/S0828282X21006243
- Myocarditis, pericarditis and cardiomyopathy after COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S1443950621011562
- Myocarditis with COVID-19 mRNA vaccines:
https://www.ahajournals.org/doi/pdf/10.1161/CIRCULATIONAHA.121.056135
- Myocarditis and pericarditis after COVID-19 vaccination: https://jamanetwork.com/journals/jama/fullarticle/2782900
- Myocarditis temporally associated with COVID-19 vaccination: https://www.ahajournals.org/doi/pdf/10.1161/CIRCULATIONAHA.121.055891.
- COVID-19 Vaccination Associated with Myocarditis in Adolescents: https://pediatrics.aappublications.org/content/pediatrics/early/2021/08/12/peds.2021-053427.full.pdf
- Acute myocarditis after administration of BNT162b2 vaccine against COVID-19:https://pubmed.ncbi.nlm.nih.gov/33994339/
- Temporal association between COVID-19 vaccine Ad26.COV2.S and acute myocarditis: case report and review of the literature: https://www.sciencedirect.com/science/article/pii/S1553838921005789
- COVID-19 vaccine-induced myocarditis: a case report with review of the literature: https://www.sciencedirect.com/science/article/pii/S1871402121002253
- Potential association between COVID-19 vaccine and myocarditis: clinical and CMR findings: https://www.sciencedirect.com/science/article/pii/S1936878X2100485X
- Recurrence of acute myocarditis temporally associated with receipt of coronavirus mRNA disease vaccine 2019 (COVID-19) in a male adolescent: https://www.sciencedirect.com/science/article/pii/S002234762100617X
- Fulminant myocarditis and systemic hyper inflammation temporally associated with BNT162b2 COVID-19 mRNA vaccination in two patients: https://www.sciencedirect.com/science/article/pii/S0167527321012286.
- Acute myocarditis after administration of BNT162b2 vaccine: https://www.sciencedirect.com/science/article/pii/S2214250921001530
- Lymphohistocytic myocarditis after vaccination with COVID-19 Ad26.COV2.S viral vector: https://www.sciencedirect.com/science/article/pii/S2352906721001573
- Myocarditis following vaccination with BNT162b2 in a healthy male: https://www.sciencedirect.com/science/article/pii/S0735675721005362
- Acute myocarditis after Comirnaty (Pfizer) vaccination in a healthy male with previous SARS-CoV-2 infection: https://www.sciencedirect.com/science/article/pii/S1930043321005549
- Acute myocarditis after vaccination with SARS-CoV-2 mRNA-1273 mRNA: https://www.sciencedirect.com/science/article/pii/S2589790X21001931
- Acute myocarditis after SARS-CoV-2 vaccination in a 24-year-old man: https://www.sciencedirect.com/science/article/pii/S0870255121003243
- A series of patients with myocarditis after vaccination against SARS-CoV-2 with mRNA-1279 and BNT162b2: https://www.sciencedirect.com/science/article/pii/S1936878X21004861
- COVID-19 mRNA vaccination and myocarditis: https://pubmed.ncbi.nlm.nih.gov/34268277/
- COVID-19 vaccine and myocarditis: https://pubmed.ncbi.nlm.nih.gov/34399967/
- Epidemiology and clinical features of myocarditis/pericarditis before the introduction of COVID-19 mRNA vaccine in Korean children: a multicenter study https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resourc e/en/covidwho-1360706.
- COVID-19 vaccines and myocarditis: https://pubmed.ncbi.nlm.nih.gov/34246566/
- Myocarditis and other cardiovascular complications of COVID-19 mRNA-based COVID-19 vaccines https://www.cureus.com/articles/61030-myocarditis-and-othercardiovascular-complications-of-the-mrna-based-covid-19-vaccines
- Myocarditis, pericarditis, and cardiomyopathy after COVID-19 vaccination: https://
pubmed.ncbi.nlm.nih.gov/34340927/
- Myocarditis with covid-19 mRNA vaccines: https://www.ahajournals.org/doi/10.1161/
CIRCULATIONAHA.121.056135
- Association of myocarditis with COVID-19 mRNA vaccine in children: https://media.jamanetwork.com/news-item/association-of-myocarditis-with-mrna-co vid-19-vaccine-in-children/
- Association of myocarditis with COVID-19 messenger RNA vaccine BNT162b2 in a case series of children: https://jamanetwork.com/journals/jamacardiology/fullarticle/2783052
- Myocarditis after immunization with COVID-19 mRNA vaccines in members of the U.S. military: https://jamanetwork.com/journals/jamacardiology/fullarticle/2781601%5C
- Myocarditis occurring after immunization with COVID-19 mRNA-based COVID-19 vaccines: https://jamanetwork.com/journals/jamacardiology/fullarticle/2781600
- Myocarditis following immunization with Covid-19 mRNA: https://www.nejm.org/doi/full/10.1056/NEJMc2109975
- Patients with acute myocarditis after vaccination withCOVID-19 mRNA: https://jamanetwork.com/journals/jamacardiology/fullarticle/2781602
- Myocarditis associated with vaccination with COVID-19 mRNA: https://pubs.rsna.org/doi/10.1148/radiol.2021211430
- Symptomatic Acute Myocarditis in 7 Adolescents after Pfizer-BioNTech COVID-19 Vaccination: https://pediatrics.aappublications.org/content/148/3/e2021052478
- Cardiovascular magnetic resonance imaging findings in young adult patients with acute myocarditis after COVID-19 mRNA vaccination: a case series: https://jcmronline.biomedcentral.com/articles/10.1186/s12968-021-00795-4
- Clinical Guidance for Young People with Myocarditis and Pericarditis after Vaccination with COVID-19 mRNA: https://www.cps.ca/en/documents/position/clinical-guidance-for-youth-with-myocarditis-and-pericarditis
- Cardiac imaging of acute myocarditis after vaccination with COVID-19 mRNA: https://pubmed.ncbi.nlm.nih.gov/34402228/
- Case report: acute myocarditis after second dose of mRNA-1273 SARS-CoV-2 mRNA vaccine: https://academic.oup.com/ehjcr/article/5/8/ytab319/6339567
- Myocarditis / pericarditis associated with COVID-19 vaccine: https://science.gc.ca/eic/site/063.nsf/eng/h_98291.html
- The new COVID-19 mRNA vaccine platform and myocarditis: clues to the possible underlying mechanism: https://pubmed.ncbi.nlm.nih.gov/34312010/
- Myocarditis associated with COVID-19 vaccination: echocardiographic, cardiac tomography, and magnetic resonance imaging findings: https://www.ahajournals.org/doi/10.1161/CIRCIMAGING.121.013236
- In-depth evaluation of a case of presumed myocarditis after the second dose of
COVID-19 mRNA vaccine: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.121.056038
- Occurrence of acute infarct-like myocarditis after COVID-19 vaccination: just an accidental coincidence or rather a vaccination-associated autoimmune myocarditis?:https://pubmed.ncbi.nlm.nih.gov/34333695/
- Recurrence of acute myocarditis temporally associated with receipt of coronavirus mRNA disease vaccine 2019 (COVID-19) in a male adolescent: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8216855/
- Myocarditis after SARS-CoV-2 vaccination: a vaccine-induced reaction?: https://pubmed.ncbi.nlm.nih.gov/34118375/
- Self-limited myocarditis presenting with chest pain and ST-segment elevation in adolescents after vaccination with the BNT162b2 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34180390/
- Biopsy-proven lymphocytic myocarditis after first COVID-19 mRNA vaccination in a 40-year-old man: case report: https://pubmed.ncbi.nlm.nih.gov/34487236/
- Myocarditis and other cardiovascular complications of mRNA-based COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34277198/
- Case report: acute myocarditis after second dose of SARS-CoV-2 mRNA-1273 vaccine mRNA-1273: https://pubmed.ncbi.nlm.nih.gov/34514306/
- Acute myocardial infarction within 24 hours after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34364657/.
- fulminant myocarditis and systemic hyperinflammation temporally associated with BNT162b2 COVID-19 mRNA vaccination in two patients: https://pubmed.ncbi.nlm.nih.gov/34416319/.
- Lymphohistocytic myocarditis after vaccination with the COVID-19 viral vector Ad26.COV2.S: https://pubmed.ncbi.nlm.nih.gov/34514078/
- Myocarditis associated with SARS-CoV-2 mRNA vaccination in children aged 12 to 17 years: stratified analysis of a national database: https://www.medrxiv.org/content/10.1101/2021.08.30.21262866v1
- A report of myocarditis adverse events in the U.S. Vaccine Adverse Event Reporting System. (VAERS) in association with COVID-19 injectable biologics: https://pubmed.ncbi.nlm.nih.gov/34601006/
- This study concludes that: “The vaccine was associated with an excess risk of myocarditis (1 to 5 events per 100,000 persons). The risk of this potentially serious adverse event and of many other serious adverse events increased substantially after SARS-CoV-2 infection”: https://www.nejm.org/doi/full/10.1056/NEJMoa2110475
- Myocarditis associated with SARS-CoV-2 mRNA vaccination in children aged 12 to 17 years: stratified analysis of a national database: https://www.medrxiv.org/content/10.1101/2021.08.30.21262866v1.
- Epidemiology of acute myocarditis/pericarditis in Hong Kong adolescents after covaccination: https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciab989/644 5179.
- Myocarditis after 2019 coronavirus disease mRNA vaccine: a case series and determination of incidence rate: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab926/6420408
- Myocarditis and pericarditis after COVID-19 vaccination: inequalities in age and vaccine types: https://www.mdpi.com/2075-4426/11/11/1106
- Epidemiology and clinical features of myocarditis/pericarditis before the introduction of COVID-19 mRNA vaccine in Korean children: a multicenter study: https://pubmed.ncbi.nlm.nih.gov/34402230/
- Shedding light on post-vaccination myocarditis and pericarditis in COVID-19 and non-COVID-19 vaccine recipients: https://pubmed.ncbi.nlm.nih.gov/34696294/
- Myocarditis Following mRNA COVID-19 Vaccine: https://journals.lww.com/pec-online/Abstract/2021/11000/Myocarditis_Following_ mRNA_COVID_19_Vaccine.9.aspx.
- Myocarditis following BNT162b2 mRNA Covid-19 mRNA vaccine in Israel: https://pubmed.ncbi.nlm.nih.gov/34614328/.
- Myocarditis, pericarditis, and cardiomyopathy following COVID-19 vaccination: https://www.heartlungcirc.org/article/S1443-9506(21)01156-2/fulltext
- Myocarditis and other cardiovascular complications of COVID-19 mRNA-based COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34277198/
- Possible Association Between COVID-19 Vaccine and Myocarditis: Clinical and CMR Findings: https://pubmed.ncbi.nlm.nih.gov/34246586/
- Hypersensitivity Myocarditis and COVID-19 Vaccines: https://pubmed.ncbi.nlm.nih.gov/34856634/.
- Severe myocarditis associated with COVID-19 vaccine: zebra or unicorn?: https://www.internationaljournalofcardiology.com/article/S0167-5273(21)01477-7/fulltext.
- Acute myocardial infarction and myocarditis after COVID-19 vaccination: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8522388/
- Myocarditis after Covid-19 vaccination in a large healthcare organization: https://www.nejm.org/doi/10.1056/NEJMoa2110737
- Association of myocarditis with COVID-19 messenger RNA BNT162b2 vaccine in a case series of children: https://jamanetwork.com/journals/jamacardiology/fullarticle/2783052
- Clinical suspicion of myocarditis temporally related to COVID-19 vaccination in adolescents and young adults: https://www.ahajournals.org/doi/abs/10.1161/CIRCULATIONAHA.121.056583?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed
- STEMI mimicry: focal myocarditis in an adolescent patient after COVID-19 mRNA vaccination:. https://pubmed.ncbi.nlm.nih.gov/34756746/
- Myocarditis and pericarditis in association with COVID-19 mRNA vaccination: cases from a regional pharmacovigilance center: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8587334/
- Myocarditis after COVID-19 mRNA vaccines: https://pubmed.ncbi.nlm.nih.gov/34546329/.
- Patients with acute myocarditis after COVID-19 mRNA vaccination:. https://jamanetwork.com/journals/jamacardiology/fullarticle/2781602.
- Myocarditis after COVID-19 vaccination: a case series: https://www.sciencedirect.com/science/article/pii/S0264410X21011725?via%3Dihub.
- Myocarditis associated with COVID-19 vaccination in adolescents: https://publications.aap.org/pediatrics/article/148/5/e2021053427/181357
- Myocarditis findings on cardiac magnetic resonance imaging after vaccination with COVID-19 mRNA in adolescents:. https://pubmed.ncbi.nlm.nih.gov/34704459/
- Myocarditis after COVID-19 vaccination: magnetic resonance imaging study: https://academic.oup.com/ehjcimaging/advance-article/doi/10.1093/ehjci/jeab230/6 421640.
- Acute myocarditis after administration of the second dose of BNT162b2 COVID-19 vaccine: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8599115/
- Myocarditis after COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S2352906721001603
- Case report: probable myocarditis after Covid-19 mRNA vaccine in a patient with arrhythmogenic left ventricular cardiomyopathy: https://pubmed.ncbi.nlm.nih.gov/34712717/.
- Acute myocarditis after administration of BNT162b2 vaccine against COVID-19: https://www.revespcardiol.org/en-linkresolver-acute-myocarditis-after-administrationbnt162b2-
S188558572100133X.
- Myocarditis associated with COVID-19 mRNA vaccination: https://pubs.rsna.org/doi/10.1148/radiol.2021211430
- Acute myocarditis after COVID-19 vaccination: a case report: https://www.sciencedirect.com/science/article/pii/S0248866321007098
- Acute myopericarditis after COVID-19 vaccination in adolescents:. https://pubmed.ncbi.nlm.nih.gov/34589238/.
- Perimyocarditis in adolescents after Pfizer-BioNTech COVID-19 vaccination: https://academic.oup.com/jpids/article/10/10/962/6329543.
- Acute myocarditis associated with anti-COVID-19 vaccination: https://ecevr.org/DOIx.php?id=10.7774/cevr.2021.10.2.196.
- Myocarditis associated with COVID-19 vaccination: echocardiographic, cardiac CT, and MRI findings:. https://pubmed.ncbi.nlm.nih.gov/34428917/.
- Acute symptomatic myocarditis in 7 adolescents after Pfizer-BioNTech COVID-19 vaccination:. https://pubmed.ncbi.nlm.nih.gov/34088762/.
- Myocarditis and pericarditis in adolescents after first and second doses of COVID-19 mRNA vaccines:. https://academic.oup.com/ehjqcco/advance-article/doi/10.1093/ehjqcco/qcab090/64 42104.
- COVID 19 vaccine for adolescents. Concern for myocarditis and pericarditis: https://www.mdpi.com/2036-7503/13/3/61.
- Cardiac imaging of acute myocarditis after vaccination with COVID-19 mRNA: https://pubmed.ncbi.nlm.nih.gov/34402228/
100.Myocarditis temporally associated with COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34133885/
101.Acute myocarditis associated with COVID-19 vaccination: report of a case: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8639400/
102.Myocarditis following vaccination with COVID-19 messenger RNA: a Japanese case series: https://pubmed.ncbi.nlm.nih.gov/34840235/.
103.Myocarditis in the setting of a recent COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34712497/.
104.Acute myocarditis after a second dose of COVID-19 mRNA vaccine: report of two cases: https://www.clinicalimaging.org/article/S0899-7071(21)00265-5/fulltext.
105.Prevalence of thrombocytopenia, antiplatelet factor 4 antibodies, and elevated Ddimer in Thais after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34568726/
106.Epidemiology of acute myocarditis/pericarditis in Hong Kong adolescents after covaccination: https://academic.oup.com/cid/advance-article-abstract/doi/10.1093/cid/ciab989/6445179
107.Myocarditis after 2019 coronavirus disease mRNA vaccine: a case series and incidence rate determination: https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab926/6420408.
108.Myocarditis and pericarditis after COVID-19 vaccination: inequalities in age and vaccine types: https://www.mdpi.com/2075-4426/11/11/1106
109.Epidemiology and clinical features of myocarditis/pericarditis before the introduction of COVID-19 mRNA vaccine in Korean children: a multicenter study: https://pubmed.ncbi.nlm.nih.gov/34402230/
110.Shedding light on post-vaccination myocarditis and pericarditis in COVID-19 and non-COVID-19 vaccine recipients: https://pubmed.ncbi.nlm.nih.gov/34696294/
112.Myocarditis-induced sudden death after BNT162b2 COVID-19 mRNA vaccination in Korea: case report focusing on histopathological findings: https://pubmed.ncbi.nlm.nih.gov/34664804/
113.Acute myocarditis after vaccination with COVID-19 mRNA in adults aged 18 years or older: https://pubmed.ncbi.nlm.nih.gov/34605853/
114.Recurrence of acute myocarditis temporally associated with receipt of the 2019 coronavirus mRNA disease vaccine (COVID-19) in an adolescent male: https://pubmed.ncbi.nlm.nih.gov/34166671/
115.Young male with myocarditis after mRNA-1273 coronavirus disease-2019 (COVID-19) mRNA vaccination: https://pubmed.ncbi.nlm.nih.gov/34744118/
116.Acute myocarditis after SARS-CoV-2 vaccination in a 24-year-old male: https://pubmed.ncbi.nlm.nih.gov/34334935/.
117.Ga-DOTATOC digital PET images of inflammatory cell infiltrates in myocarditis after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34746968/
118.Occurrence of acute infarct-like myocarditis after vaccination with COVID-19: just an accidental coincidence or rather a vaccination-associated autoimmune myocarditis?”:https://pubmed.ncbi.nlm.nih.gov/34333695/.
119.Self-limited myocarditis presenting with chest pain and ST-segment elevation in adolescents after vaccination with BNT162b2 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34180390/
120.Myocarditis Following Immunization with COVID-19 mRNA Vaccines in Members of the U.S. Military: https://pubmed.ncbi.nlm.nih.gov/34185045/
121.Myocarditis after BNT162b2 vaccination in a healthy male: https://pubmed.ncbi.nlm.nih.gov/34229940/
122.Acute myocarditis after SARS-CoV-2 mRNA-1273 mRNA vaccination: https://pubmed.ncbi.nlm.nih.gov/34308326/.
123.Biopsy-proven lymphocytic myocarditis after first vaccination with COVID-19 mRNA in a 40-year-old man: case report: https://pubmed.ncbi.nlm.nih.gov/34487236/
124.Multimodality imaging and histopathology in a young man presenting with fulminant lymphocytic myocarditis and cardiogenic shock after vaccination with mRNA-1273: https://pubmed.ncbi.nlm.nih.gov/34848416/
125.Acute myocarditis after Comirnaty vaccination in a healthy male with previous SARS-CoV-2 infection: https://pubmed.ncbi.nlm.nih.gov/34367386/
126.Acute myocarditis in a young adult two days after vaccination with Pfizer: https://pubmed.ncbi.nlm.nih.gov/34709227/
127.Case report: acute fulminant myocarditis and cardiogenic shock after messenger RNA coronavirus vaccination in 2019 requiring extracorporeal cardiopulmonary resuscitation: https://pubmed.ncbi.nlm.nih.gov/34778411/
128.Acute myocarditis after 2019 coronavirus disease vaccination: https://pubmed.ncbi.nlm.nih.gov/34734821/
129.A series of patients with myocarditis after vaccination against SARS-CoV-2 with mRNA-1279 and BNT162b2: https://pubmed.ncbi.nlm.nih.gov/34246585/
130.Acute myocarditis defined after vaccination with 2019 mRNA of coronavirus disease: https://pubmed.ncbi.nlm.nih.gov/34866122/
131.Biventricular systolic dysfunction in acute myocarditis after SARS-CoV-2 mRNA-1273 vaccination: https://pubmed.ncbi.nlm.nih.gov/34601566/
132.Myocarditis following COVID-19 vaccination: MRI study: https://pubmed.ncbi.nlm.nih.gov/34739045/.
133.Acute myocarditis after COVID-19 vaccination: case report: https://docs.google.com/document/d/1Hc4bh_qNbZ7UVm5BLxkRdMPnnI9zcCsl/e
134.Association of myocarditis with COVID-19 messenger RNA BNT162b2 vaccine COVID-19 in a case series of children: https://pubmed.ncbi.nlm.nih.gov/34374740/
135.Clinical suspicion of myocarditis temporally related to COVID-19 vaccination in adolescents and young adults: https://pubmed.ncbi.nlm.nih.gov/34865500/
136.Myocarditis following vaccination with Covid-19 in a large healthcare organization: https://pubmed.ncbi.nlm.nih.gov/34614329/
137.Myocarditis and pericarditis in adolescents after the first and second doses of COVID-19 mRNA vaccines: https://pubmed.ncbi.nlm.nih.gov/34849667/
138.Myocarditis after SARS-CoV-2 mRNA vaccination, a case series: https://pubmed.ncbi.nlm.nih.gov/34396358/.
139.Epidemiology of myocarditis and pericarditis following mRNA vaccines in Ontario, Canada: by vaccine product, schedule, and interval: https://www.medrxiv.org/content/10.1101/2021.12.02.21267156v1
140.Acute myocardial infarction and myocarditis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34586408/
141.Abbate, A., Gavin, J., Madanchi, N., Kim, C., Shah, P. R., Klein, K., . . . Danielides, S. (2021). Fulminant myocarditis and systemic hyperinflammation temporally associated with BNT162b2 mRNA COVID-19 vaccination in two patients. Int J Cardiol, 340, 119-121. doi:10.1016/j.ijcard.2021.08.018. https://www.ncbi.nlm.nih.gov/pubmed/34416319
142.Abu Mouch, S., Roguin, A., Hellou, E., Ishai, A., Shoshan, U., Mahamid, L., .Berar Yanay, N. (2021). Myocarditis following COVID-19 mRNA vaccination. Vaccine, 39(29), 3790-3793. doi:10.1016/j.vaccine.2021.05.087. https://www.ncbi.nlm.nih.gov/pubmed/34092429
143.Albert, E., Aurigemma, G., Saucedo, J., & Gerson, D. S. (2021). Myocarditis following COVID-19 vaccination. Radiol Case Rep, 16(8), 2142-2145. doi:10.1016/j.radcr.2021.05.033. https://www.ncbi.nlm.nih.gov/pubmed/34025885
144.Aye, Y. N., Mai, A. S., Zhang, A., Lim, O. Z. H., Lin, N., Ng, C. H., . . . Chew, N. W. S. (2021). Acute Myocardial Infarction and Myocarditis following COVID-19 Vaccination. QJM. doi:10.1093/qjmed/hcab252. https://www.ncbi.nlm.nih.gov/pubmed/34586408
145.Azir, M., Inman, B., Webb, J., & Tannenbaum, L. (2021). STEMI Mimic: Focal Myocarditis in an Adolescent Patient After mRNA COVID-19 Vaccine. J Emerg Med, 61(6), e129-e132. doi:10.1016/j.jemermed.2021.09.017. https://www.ncbi.nlm.nih.gov/pubmed/34756746
146.Bozkurt, B., Kamat, I., & Hotez, P. J. (2021). Myocarditis With COVID-19 mRNA Vaccines. Circulation, 144(6), 471-484. doi:10.1161/CIRCULATIONAHA.121.056135. https://www.ncbi.nlm.nih.gov/pubmed/34281357
147.Calcaterra, G., Mehta, J. L., de Gregorio, C., Butera, G., Neroni, P., Fanos, V., & Bassareo, P. P. (2021). COVID 19 Vaccine for Adolescents. Concern about Myocarditis and Pericarditis. Pediatr Rep, 13(3), 530-533. doi:10.3390/
pediatric13030061. https://www.ncbi.nlm.nih.gov/pubmed/34564344
148.Chamling, B., Vehof, V., Drakos, S., Weil, M., Stalling, P., Vahlhaus, C., . . . Yilmaz, A. (2021). Occurrence of acute infarct-like myocarditis following COVID-19 vaccination: just an accidental co-incidence or rather vaccination-associated autoimmune myocarditis? Clin Res Cardiol, 110(11), 1850-1854. doi:10.1007/s00392-021-01916-w. https://www.ncbi.nlm.nih.gov/pubmed/34333695
149.Chelala, L., Jeudy, J., Hossain, R., Rosenthal, G., Pietris, N., & White, C. (2021). Cardiac MRI Findings of Myocarditis After COVID-19 mRNA Vaccination in Adolescents. AJR Am J Roentgenol. doi:10.2214/AJR.21.26853. https://www.ncbi.nlm.nih.gov/pubmed/34704459
150.Choi, S., Lee, S., Seo, J. W., Kim, M. J., Jeon, Y. H., Park, J. H., . . . Yeo, N. S. (2021). Myocarditis-induced Sudden Death after BNT162b2 mRNA COVID-19 Vaccination in Korea: Case Report Focusing on Histopathological Findings. J Korean Med Sci, 36(40), e286. doi:10.3346/jkms.2021.36.e286. https://www.ncbi.nlm.nih.gov/pubmed/34664804
151.Chua, G. T., Kwan, M. Y. W., Chui, C. S. L., Smith, R. D., Cheung, E. C., Tian, T., . Ip, P. (2021). Epidemiology of Acute Myocarditis/Pericarditis in Hong Kong Adolescents Following Comirnaty Vaccination. Clin Infect Dis. doi:10.1093/cid/ciab989. https://www.ncbi.nlm.nih.gov/pubmed/34849657
152.Clarke, R., & Ioannou, A. (2021). Should T2 mapping be used in cases of recurrent myocarditis to differentiate between the acute inflammation and chronic scar? J Pediatr. doi:10.1016/j.jpeds.2021.12.026. https://www.ncbi.nlm.nih.gov/pubmed/34933012
153.Das, B. B., Moskowitz, W. B., Taylor, M. B., & Palmer, A. (2021). Myocarditis and Pericarditis Following mRNA COVID-19 Vaccination: What Do We Know So Far? Children (Basel), 8(7). doi:10.3390/children8070607. https://www.ncbi.nlm.nih.gov/ pubmed/34356586
154.Dickey, J. B., Albert, E., Badr, M., Laraja, K. M., Sena, L. M., Gerson, D. S., Aurigemma, G. P. (2021). A Series of Patients With Myocarditis Following SARSCoV-2 Vaccination With mRNA-1279 and BNT162b2. JACC Cardiovasc Imaging,14(9), 1862-1863. doi:10.1016/j.jcmg.2021.06.003. https://www.ncbi.nlm.nih.gov/pubmed/34246585
155.Ehrlich, P., Klingel, K., Ohlmann-Knafo, S., Huttinger, S., Sood, N., Pickuth, D., & Kindermann, M. (2021). Biopsy-proven lymphocytic myocarditis following first mRNA COVID-19 vaccination in a 40-year-old male: case report. Clin Res Cardiol, 110(11), 1855-1859. doi:10.1007/s00392-021-01936-6. https://www.ncbi.nlm.nih.gov/pubmed/34487236
156.Facetti, S., Giraldi, M., Vecchi, A. L., Rogiani, S., & Nassiacos, D. (2021). [Acute myocarditis in a young adult two days after Pfizer vaccination]. G Ital Cardiol (Rome), 22(11), 891-893. doi:10.1714/3689.36746. https://www.ncbi.nlm.nih.gov/pubmed/34709227
157.Foltran, D., Delmas, C., Flumian, C., De Paoli, P., Salvo, F., Gautier, S., . Montastruc, F. (2021). Myocarditis and Pericarditis in Adolescents after First and Second doses of mRNA COVID-19 Vaccines. Eur Heart J Qual Care Clin Outcomes. doi:10.1093/ehjqcco/qcab090. https://www.ncbi.nlm.nih.gov/pubmed/34849667
158.Gargano, J. W., Wallace, M., Hadler, S. C., Langley, G., Su, J. R., Oster, M. E., . Oliver, S. E. (2021). Use of mRNA COVID-19 Vaccine After Reports of Myocarditis Among Vaccine Recipients: Update from the Advisory Committee on Immunization Practices – United States, June 2021. MMWR Morb Mortal Wkly Rep, 70(27), 977-982. doi:10.15585/mmwr.mm7027e2. https://www.ncbi.nlm.nih.gov/pubmed/34237049
159.Gautam, N., Saluja, P., Fudim, M., Jambhekar, K., Pandey, T., & Al’Aref, S. (2021). A Late Presentation of COVID-19 Vaccine-Induced Myocarditis. Cureus, 13(9), e17890. doi:10.7759/cureus.17890. https://www.ncbi.nlm.nih.gov/pubmed/34660088
160.Gellad, W. F. (2021). Myocarditis after vaccination against covid-19. BMJ, 375, n3090. doi:10.1136/bmj.n3090. https://www.ncbi.nlm.nih.gov/pubmed/34916217
161.In brief: Myocarditis with the Pfizer/BioNTech and Moderna COVID-19 vaccines. (2021). Med Lett Drugs Ther, 63(1629), e9. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/34544112https://www.ncbi.nlm.nih.gov/pubmed/3454412
162.Ioannou, A. (2021a). Myocarditis should be considered in those with a troponin rise and unobstructed coronary arteries following Pfizer-BioNTech COVID-19 vaccination. QJM. doi:10.1093/qjmed/hcab231. https://www.ncbi.nlm.nih.gov/pubmed/34463755
163.Ioannou, A. (2021b). T2 mapping should be utilised in cases of suspected myocarditis to confirm an acute inflammatory process. QJM. doi:10.1093/qjmed/hcab326. https://www.ncbi.nlm.nih.gov/pubmed/34931681
164.Isaak, A., Feisst, A., & Luetkens, J. A. (2021). Myocarditis Following COVID-19 Vaccination. Radiology, 301(1), E378-E379. doi:10.1148/radiol.2021211766. https://www.ncbi.nlm.nih.gov/pubmed/34342500
165.Istampoulouoglou, I., Dimitriou, G., Spani, S., Christ, A., Zimmermanns, B., Koechlin, S., . . . Leuppi-Taegtmeyer, A. B. (2021). Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: cases from a regional
pharmacovigilance centre. Glob Cardiol Sci Pract, 2021(3), e202118. doi:10.21542/gcsp.2021.18. https://www.ncbi.nlm.nih.gov/pubmed/34805376
166.Jain, S. S., Steele, J. M., Fonseca, B., Huang, S., Shah, S., Maskatia, S. A., Grosse-Wortmann, L. (2021). COVID-19 Vaccination-Associated Myocarditis in Adolescents. Pediatrics, 148(5). doi:10.1542/peds.2021-053427. https://www.ncbi.nlm.nih.gov/pubmed/34389692
167.Kaneta, K., Yokoi, K., Jojima, K., Kotooka, N., & Node, K. (2021). Young Male With Myocarditis Following mRNA-1273 Vaccination Against Coronavirus Disease-2019 (COVID-19). Circ J. doi:10.1253/circj.CJ-21-0818. https://www.ncbi.nlm.nih.gov/pubmed/34744118
168.Kaul, R., Sreenivasan, J., Goel, A., Malik, A., Bandyopadhyay, D., Jin, C., . . . Panza, J. A. (2021). Myocarditis following COVID-19 vaccination. Int J Cardiol Heart Vasc, 36, 100872. doi:10.1016/j.ijcha.2021.100872. https://www.ncbi.nlm.nih.gov/pubmed/34568540
169.Kim, H. W., Jenista, E. R., Wendell, D. C., Azevedo, C. F., Campbell, M. J., Darty, S. N., . . . Kim, R. J. (2021). Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol, 6(10), 1196-1201. doi:10.1001/jamacardio. 2021.2828. https://www.ncbi.nlm.nih.gov/pubmed/34185046
170.Kim, I. C., Kim, H., Lee, H. J., Kim, J. Y., & Kim, J. Y. (2021). Cardiac Imaging of Acute Myocarditis Following COVID-19 mRNA Vaccination. J Korean Med Sci, 36(32), e229. doi:10.3346/jkms.2021.36.e229. https://www.ncbi.nlm.nih.gov/pubmed/34402228
171.King, W. W., Petersen, M. R., Matar, R. M., Budweg, J. B., Cuervo Pardo, L., & Petersen, J. W. (2021). Myocarditis following mRNA vaccination against SARSCoV-2, a case series. Am Heart J Plus, 8, 100042. doi:10.1016/j.ahjo.2021.100042. https://www.ncbi.nlm.nih.gov/pubmed/34396358
172.Kwan, M. Y. W., Chua, G. T., Chow, C. B., Tsao, S. S. L., To, K. K. W., Yuen, K. Y., .. Ip, P. (2021). mRNA COVID vaccine and myocarditis in adolescents. Hong Kong Med J, 27(5), 326-327. doi:10.12809/hkmj215120. https://www.ncbi.nlm.nih.gov/pubmed/34393110
173.Lee, E., Chew, N. W. S., Ng, P., & Yeo, T. J. (2021). Reply to “Letter to the editor: Myocarditis should be considered in those with a troponin rise and unobstructed coronary arteries following PfizerBioNTech COVID-19 vaccination”. QJM. doi: 10.1093/qjmed/hcab232. https://www.ncbi.nlm.nih.gov/pubmed/34463770
174.Levin, D., Shimon, G., Fadlon-Derai, M., Gershovitz, L., Shovali, A., Sebbag, A.,Gordon, B. (2021). Myocarditis following COVID-19 vaccination – A case series. Vaccine, 39(42), 6195-6200. doi:10.1016/j.vaccine.2021.09.004. https://www.ncbi.nlm.nih.gov/pubmed/34535317
175.Li, M., Yuan, J., Lv, G., Brown, J., Jiang, X., & Lu, Z. K. (2021). Myocarditis and Pericarditis following COVID-19 Vaccination: Inequalities in Age and Vaccine Types. J Pers Med, 11(11). doi:10.3390/jpm11111106. https://www.ncbi.nlm.nih.gov/pubmed/34834458
176.Lim, Y., Kim, M. C., Kim, K. H., Jeong, I. S., Cho, Y. S., Choi, Y. D., & Lee, J. E. (2021). Case Report: Acute Fulminant Myocarditis and Cardiogenic Shock After Messenger RNA Coronavirus Disease 2019 Vaccination Requiring Extracorporeal Cardiopulmonary Resuscitation. Front Cardiovasc Med, 8, 758996. doi:10.3389/fcvm.2021.758996. https://www.ncbi.nlm.nih.gov/pubmed/34778411
177.Luk, A., Clarke, B., Dahdah, N., Ducharme, A., Krahn, A., McCrindle, B., .McDonald, M. (2021). Myocarditis and Pericarditis After COVID-19 mRNA Vaccination: Practical Considerations for Care Providers. Can J Cardiol, 37(10), 1629-1634. doi:10.1016/j.cjca.2021.08.001. https://www.ncbi.nlm.nih.gov/pubmed/34375696
178.Mevorach, D., Anis, E., Cedar, N., Bromberg, M., Haas, E. J., Nadir, E., . . . Alroy-Preis, S. (2021). Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med, 385(23), 2140-2149. doi:10.1056/NEJMoa2109730. https://www.ncbi.nlm.nih.gov/pubmed/34614328
179.Minocha, P. K., Better, D., Singh, R. K., & Hoque, T. (2021). Recurrence of Acute Myocarditis Temporally Associated with Receipt of the mRNA Coronavirus Disease 2019 (COVID-19) Vaccine in a Male Adolescent. J Pediatr, 238, 321-323. doi: 10.1016/j.jpeds.2021.06.035. https://www.ncbi.nlm.nih.gov/pubmed/34166671
180.Montgomery, J., Ryan, M., Engler, R., Hoffman, D., McClenathan, B., Collins, L.,Cooper, L. T., Jr. (2021). Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol, 6(10), 1202-1206. doi: 10.1001/jamacardio.2021.2833. https://www.ncbi.nlm.nih.gov/pubmed/34185045
181.Murakami, Y., Shinohara, M., Oka, Y., Wada, R., Noike, R., Ohara, H., . . . Ikeda, T. (2021). Myocarditis Following a COVID-19 Messenger RNA Vaccination: A Japanese Case Series. Intern Med. doi:10.2169/internalmedicine.8731-21. https://www.ncbi.nlm.nih.gov/pubmed/34840235
182.Nagasaka, T., Koitabashi, N., Ishibashi, Y., Aihara, K., Takama, N., Ohyama, Y., . Kaneko, Y. (2021). Acute Myocarditis Associated with COVID-19 Vaccination: A Case Report. J Cardiol Cases. doi:10.1016/j.jccase.2021.11.006. https://www.ncbi.nlm.nih.gov/pubmed/34876937
183.Park, H., Yun, K. W., Kim, K. R., Song, S. H., Ahn, B., Kim, D. R., . . . Kim, Y. J. (2021). Epidemiology and Clinical Features of Myocarditis/Pericarditis before the Introduction of mRNA COVID-19 Vaccine in Korean Children: a Multicenter Study. J Korean Med Sci, 36(32), e232. doi:10.3346/jkms.2021.36.e232. https://www.ncbi.nlm.nih.gov/pubmed/34402230
184.Park, J., Brekke, D. R., & Bratincsak, A. (2021). Self-limited myocarditis presenting with chest pain and ST segment elevation in adolescents after vaccination with the BNT162b2 mRNA vaccine. Cardiol Young, 1-4. doi:10.1017/S1047951121002547. https://www.ncbi.nlm.nih.gov/pubmed/34180390
185.Patel, Y. R., Louis, D. W., Atalay, M., Agarwal, S., & Shah, N. R. (2021). Cardiovascular magnetic resonance findings in young adult patients with acute myocarditis following mRNA COVID-19 vaccination: a case series. J Cardiovasc Magn Reson, 23(1), 101. doi:10.1186/s12968-021-00795-4. https://www.ncbi.nlm.nih.gov/pubmed/34496880
186.Patone, M., Mei, X. W., Handunnetthi, L., Dixon, S., Zaccardi, F., Shankar-Hari, M., . . . Hippisley-Cox, J. (2021). Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. doi:10.1038/s41591-021-01630-0. https://www.ncbi.nlm.nih.gov/pubmed/34907393
187.Patrignani, A., Schicchi, N., Calcagnoli, F., Falchetti, E., Ciampani, N., Argalia, G., & Mariani, A. (2021). Acute myocarditis following Comirnaty vaccination in a healthy man with previous SARS-CoV-2 infection. Radiol Case Rep, 16(11), 3321-3325. doi: 10.1016/j.radcr.2021.07.082. https://www.ncbi.nlm.nih.gov/pubmed/34367386
188.Perez, Y., Levy, E. R., Joshi, A. Y., Virk, A., Rodriguez-Porcel, M., Johnson, M.,Swift, M. D. (2021). Myocarditis Following COVID-19 mRNA Vaccine: A Case Series and Incidence Rate Determination. Clin Infect Dis. doi:10.1093/cid/ciab926. https://www.ncbi.nlm.nih.gov/pubmed/34734240
189.Shiyovich, A., Witberg, G., Aviv, Y., Eisen, A., Orvin, K., Wiessman, M., . . . Hamdan, A. (2021). Myocarditis following COVID-19 vaccination: magnetic resonance imaging study. Eur Heart J Cardiovasc Imaging. doi:10.1093/ehjci/jeab230. https://www.ncbi.nlm.nih.gov/pubmed/34739045
190.Simone, A., Herald, J., Chen, A., Gulati, N., Shen, A. Y., Lewin, B., & Lee, M. S. (2021). Acute Myocarditis Following COVID-19 mRNA Vaccination in Adults Aged 18 Years or Older. JAMA Intern Med, 181(12), 1668-1670. doi:10.1001/jamainternmed. 2021.5511. https://www.ncbi.nlm.nih.gov/pubmed/34605853
191.Singer, M. E., Taub, I. B., & Kaelber, D. C. (2021). Risk of Myocarditis from COVID-19 Infection in People Under Age 20: A Population-Based Analysis. medRxiv. doi:10.1101/2021.07.23.21260998. https://www.ncbi.nlm.nih.gov/pubmed/34341797
192.Starekova, J., Bluemke, D. A., Bradham, W. S., Grist, T. M., Schiebler, M. L., & Reeder, S. B. (2021). Myocarditis Associated with mRNA COVID-19 Vaccination. Radiology, 301(2), E409-E411. doi:10.1148/radiol.2021211430. https://www.ncbi.nlm.nih.gov/pubmed/34282971
193.Sulemankhil, I., Abdelrahman, M., & Negi, S. I. (2021). Temporal association between the COVID-19 Ad26.COV2.S vaccine and acute myocarditis: A case report and literature review. Cardiovasc Revasc Med. doi:10.1016/j.carrev.2021.08.012. https://www.ncbi.nlm.nih.gov/pubmed/34420869
194.Tailor, P. D., Feighery, A. M., El-Sabawi, B., & Prasad, A. (2021). Case report: acute myocarditis following the second dose of mRNA-1273 SARS-CoV-2 vaccine. Eur Heart J Case Rep, 5(8), ytab319. doi:10.1093/ehjcr/ytab319. https://www.ncbi.nlm.nih.gov/pubmed/34514306
195.Takeda, M., Ishio, N., Shoji, T., Mori, N., Matsumoto, M., & Shikama, N. (2021). Eosinophilic Myocarditis Following Coronavirus Disease 2019 (COVID-19) Vaccination. Circ J. doi:10.1253/circj.CJ-21-0935. https://www.ncbi.nlm.nih.gov/pubmed/34955479
196.Truong, D. T., Dionne, A., Muniz, J. C., McHugh, K. E., Portman, M. A., Lambert, L. M., . . . Newburger, J. W. (2021). Clinically Suspected Myocarditis Temporally Related to COVID-19 Vaccination in Adolescents and Young Adults. Circulation. doi: 10.1161/CIRCULATIONAHA.121.056583. https://www.ncbi.nlm.nih.gov/pubmed/34865500
197.Vidula, M. K., Ambrose, M., Glassberg, H., Chokshi, N., Chen, T., Ferrari, V. A., & Han, Y. (2021). Myocarditis and Other Cardiovascular Complications of the mRNABased COVID-19 Vaccines. Cureus, 13(6), e15576. doi:10.7759/cureus.15576. https://www.ncbi.nlm.nih.gov/pubmed/34277198
198.Visclosky, T., Theyyunni, N., Klekowski, N., & Bradin, S. (2021). Myocarditis Following mRNA COVID-19 Vaccine. Pediatr Emerg Care, 37(11), 583-584. doi: 10.1097/PEC.0000000000002557. https://www.ncbi.nlm.nih.gov/pubmed/34731877
199.Watkins, K., Griffin, G., Septaric, K., & Simon, E. L. (2021). Myocarditis after BNT162b2 vaccination in a healthy male. Am J Emerg Med, 50, 815 e811-815 e812. doi:10.1016/j.ajem.2021.06.051. https://www.ncbi.nlm.nih.gov/pubmed/34229940
200.Witberg, G., Barda, N., Hoss, S., Richter, I., Wiessman, M., Aviv, Y., . . . Kornowski, R. (2021). Myocarditis after Covid-19 Vaccination in a Large Health Care Organization. N Engl J Med, 385(23), 2132-2139. doi:10.1056/NEJMoa2110737. https://www.ncbi.nlm.nih.gov/pubmed/34614329
201.In brief: Myocarditis with the Pfizer/BioNTech and Moderna COVID-19 vaccines. (2021). Med Lett Drugs Ther, 63(1629), e9.
Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/34544112https://www.ncbi.nlm.nih.gov/pubmed/
3454412
202.Ioannou, A. (2021a). Myocarditis should be considered in those with a troponin rise and unobstructed coronary arteries following Pfizer-BioNTech COVID-19 vaccination. QJM. doi:10.1093/qjmed/hcab231. https://www.ncbi.nlm.nih.gov/pubmed/34463755
203.Isaak, A., Feisst, A., & Luetkens, J. A. (2021). Myocarditis Following COVID-19 Vaccination. Radiology, 301(1), E378-E379. doi:10.1148/radiol.2021211766. https://www.ncbi.nlm.nih.gov/pubmed/34342500
204.Istampoulouoglou, I., Dimitriou, G., Spani, S., Christ, A., Zimmermanns, B., Koechlin, S., . . . Leuppi-Taegtmeyer, A. B. (2021). Myocarditis and pericarditis in association with COVID-19 mRNA-vaccination: cases from a regional
pharmacovigilance centre. Glob Cardiol Sci Pract, 2021(3), e202118. doi:10.21542/gcsp.2021.18. https://www.ncbi.nlm.nih.gov/pubmed/34805376
205.Jain, S. S., Steele, J. M., Fonseca, B., Huang, S., Shah, S., Maskatia, S. A., . Grosse-Wortmann, L. (2021). COVID-19 Vaccination-Associated Myocarditis in Adolescents. Pediatrics, 148(5). doi:10.1542/peds.2021-053427. https://www.ncbi.nlm.nih.gov/pubmed/34389692
206.Kaneta, K., Yokoi, K., Jojima, K., Kotooka, N., & Node, K. (2021). Young Male With Myocarditis Following mRNA-1273 Vaccination Against Coronavirus Disease-2019 (COVID-19). Circ J. doi:10.1253/circj.CJ-21-0818. https://www.ncbi.nlm.nih.gov/pubmed/34744118
207.Kaul, R., Sreenivasan, J., Goel, A., Malik, A., Bandyopadhyay, D., Jin, C., . . . Panza, J. A. (2021). Myocarditis following COVID-19 vaccination. Int J Cardiol Heart Vasc, 36, 100872. doi:10.1016/j.ijcha.2021.100872. https://www.ncbi.nlm.nih.gov/pubmed/34568540
208.Kim, H. W., Jenista, E. R., Wendell, D. C., Azevedo, C. F., Campbell, M. J., Darty, S. N., . . . Kim, R. J. (2021). Patients With Acute Myocarditis Following mRNA COVID-19 Vaccination. JAMA Cardiol, 6(10), 1196-1201. doi:10.1001/jamacardio. 2021.2828. https://www.ncbi.nlm.nih.gov/pubmed/34185046
209.Kim, I. C., Kim, H., Lee, H. J., Kim, J. Y., & Kim, J. Y. (2021). Cardiac Imaging of Acute Myocarditis Following COVID-19 mRNA Vaccination. J Korean Med Sci, 36(32), e229. doi:10.3346/jkms.2021.36.e229. https://www.ncbi.nlm.nih.gov/pubmed/34402228
210.King, W. W., Petersen, M. R., Matar, R. M., Budweg, J. B., Cuervo Pardo, L., & Petersen, J. W. (2021). Myocarditis following mRNA vaccination against SARSCoV-2, a case series. Am Heart J Plus, 8, 100042. doi:10.1016/j.ahjo.2021.100042. https://www.ncbi.nlm.nih.gov/pubmed/34396358
211.Kwan, M. Y. W., Chua, G. T., Chow, C. B., Tsao, S. S. L., To, K. K. W., Yuen, K. Y., . . . Ip, P. (2021). mRNA COVID vaccine and myocarditis in adolescents. Hong Kong Med J, 27(5), 326-327. doi:10.12809/hkmj215120. https://
www.ncbi.nlm.nih.gov/pubmed/34393110
212.Lee, E., Chew, N. W. S., Ng, P., & Yeo, T. J. (2021). Reply to “Letter to the editor: Myocarditis should be considered in those with a troponin rise and unobstructed coronary arteries following PfizerBioNTech COVID-19 vaccination”. QJM. doi: 10.1093/qjmed/hcab232. https://www.ncbi.nlm.nih.gov/pubmed/34463770
213.Levin, D., Shimon, G., Fadlon-Derai, M., Gershovitz, L., Shovali, A., Sebbag, A., . . .Gordon, B. (2021). Myocarditis following COVID-19 vaccination – A case series. Vaccine, 39(42), 6195-6200. doi:10.1016/j.vaccine.2021.09.004. https://www.ncbi.nlm.nih.gov/pubmed/34535317
214.Li, M., Yuan, J., Lv, G., Brown, J., Jiang, X., & Lu, Z. K. (2021). Myocarditis and Pericarditis following COVID-19 Vaccination: Inequalities in Age and Vaccine Types. J Pers Med, 11(11). doi:10.3390/jpm11111106. https://www.ncbi.nlm.nih.gov/pubmed/34834458
215.Lim, Y., Kim, M. C., Kim, K. H., Jeong, I. S., Cho, Y. S., Choi, Y. D., & Lee, J. E. (2021). Case Report: Acute Fulminant Myocarditis and Cardiogenic Shock After Messenger RNA Coronavirus Disease 2019 Vaccination Requiring Extracorporeal Cardiopulmonary Resuscitation. Front Cardiovasc Med, 8, 758996. doi:10.3389/fcvm.2021.758996. https://www.ncbi.nlm.nih.gov/pubmed/34778411
216.Luk, A., Clarke, B., Dahdah, N., Ducharme, A., Krahn, A., McCrindle, B., . . . McDonald, M. (2021). Myocarditis and Pericarditis After COVID-19 mRNA Vaccination: Practical Considerations for Care Providers. Can J Cardiol, 37(10),
1629-1634. doi:10.1016/j.cjca.2021.08.001. https://www.ncbi.nlm.nih.gov/pubmed/34375696
217.Mevorach, D., Anis, E., Cedar, N., Bromberg, M., Haas, E. J., Nadir, E., . . . Alroy-Preis, S. (2021). Myocarditis after BNT162b2 mRNA Vaccine against Covid-19 in Israel. N Engl J Med, 385(23), 2140-2149. doi:10.1056/NEJMoa2109730. https://www.ncbi.nlm.nih.gov/pubmed/34614328
218.Minocha, P. K., Better, D., Singh, R. K., & Hoque, T. (2021). Recurrence of Acute Myocarditis Temporally Associated with Receipt of the mRNA Coronavirus Disease 2019 (COVID-19) Vaccine in a Male Adolescent. J Pediatr, 238, 321-323. doi: 10.1016/j.jpeds.2021.06.035. https://www.ncbi.nlm.nih.gov/pubmed/34166671
219.Montgomery, J., Ryan, M., Engler, R., Hoffman, D., McClenathan, B., Collins, L., . . .Cooper, L. T., Jr. (2021). Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military. JAMA Cardiol, 6(10), 1202-1206. doi: 10.1001/jamacardio.2021.2833. https://www.ncbi.nlm.nih.gov/pubmed/34185045
220.Murakami, Y., Shinohara, M., Oka, Y., Wada, R., Noike, R., Ohara, H., . . . Ikeda, T. (2021). Myocarditis Following a COVID-19 Messenger RNA Vaccination: A Japanese Case Series. Intern Med. doi:10.2169/internalmedicine.8731-21. https://www.ncbi.nlm.nih.gov/pubmed/34840235
221.Nagasaka, T., Koitabashi, N., Ishibashi, Y., Aihara, K., Takama, N., Ohyama, Y., . . . Kaneko, Y. (2021). Acute Myocarditis Associated with COVID-19 Vaccination: A Case Report. J Cardiol Cases. doi:10.1016/j.jccase.2021.11.006. https://www.ncbi.nlm.nih.gov/pubmed/34876937
222.Premature myocardial infarction or side effect of COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33824804/
- Acute Myocardial Infarction Within 24 Hours After COVID-19 Vaccination: Is Kounis Syndrome the Culprit https://pubmed.ncbi.nlm.nih.gov/34702550/
224.A case of acute encephalopathy and non-ST-segment elevation myocardial infarction after vaccination with mRNA-1273: possible adverse effect: https://pubmed.ncbi.nlm.nih.gov/34703815/
- Acute myocardial infarction within 24 hours after COVID-19 vaccination: is Kounis syndrome Clinical and histopathologic spectrum of delayed adverse skin reactions after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34292611/.
226.Chouchana, L., Blet, A., Al-Khalaf, M., Kafil, T. S., Nair, G., Robblee, J., . . . Liu, P. P. (2021). Features of Inflammatory Heart Reactions Following mRNA COVID-19 Vaccination at a Global Level. Clin Pharmacol Ther. doi:10.1002/cpt.2499. https://www.ncbi.nlm.nih.gov/pubmed/34860360
- Myocarditis and other cardiovascular complications of COVID-19 mRNA-based COVID-19 vaccines https://www.cureus.com/articles/61030-myocarditis-and-othercardiovascular-complications-of-the-mrna-based-covid-19-vaccines
- Cardiovascular magnetic resonance imaging findings in young adult patients with acute myocarditis after COVID-19 mRNA vaccination: a case series: https://jcmronline.biomedcentral.com/articles/10.1186/s12968-021-00795-4
- Be alert to the risk of adverse cardiovascular events after COVID-19 vaccination: https://www.xiahepublishing.com/m/2472-0712/ERHM-2021-00033
- Myocarditis and other cardiovascular complications of mRNA-based COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34277198/
- -Diaz GA, Parsons GT, Gering SK, Meier AR, Hutchinson IV, Robicsek A. Myocarditis and Pericarditis After Vaccination for COVID-19. Jama. 2021;326(12):1210-2.
- D. Shay et al., Myocarditis occurring after immunization with mRNA-based COVID-19 vaccines, JAMA, Editorial, 06/29/2021.
- Montgomery J. et al., Myocarditis following immunization with mRNA COVID-19 vaccines in members of the US army, JAMA Cardiol., 06/29/2021.
- Surveillance of myocarditis (inflammation of the heart muscle) cases between Dec. 2020 and May 2021. News release, Israel Ministry of health June 6, 2021.
- Stepniak M., Radiologists, CDC warn of myocarditis after COVID-19 vaccination, Radiology Business, May 2021.
Μυοκαρδιακή βλάβη
- Acute myocardial injury after COVID-19 vaccination: a case report and review of current evidence from the Vaccine Adverse Event Reporting System database: https://pubmed.ncbi.nlm.nih.gov/34219532/
- Deb, A., Abdelmalek, J., Iwuji, K., & Nugent, K. (2021). Acute Myocardial Injury Following COVID-19 Vaccination: A Case Report and Review of Current Evidence from Vaccine Adverse Events Reporting System Database. J Prim Care Community Health, 12, 21501327211029230. doi:10.1177/21501327211029230. https://www.ncbi.nlm.nih.gov/pubmed/34219532
Περικαρδίτιδα
- Myocarditis and pericarditis after vaccination with COVID-19 mRNA: practical considerations for care providers: https://www.sciencedirect.com/science/article/pii/S0828282X21006243
- Myocarditis, pericarditis and cardiomyopathy after COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S1443950621011562
- Myocarditis and pericarditis after COVID-19 vaccination: https://jamanetwork.com/journals/jama/fullarticle/2782900
- Pericarditis after administration of BNT162b2 mRNA COVID-19 mRNA vaccine: https://www.sciencedirect.com/science/article/pii/S1885585721002218
- Epidemiology and clinical features of myocarditis/pericarditis before the introduction of COVID-19 mRNA vaccine in Korean children: a multicenter study https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resourc e/en/covidwho-1360706.
- Myocarditis, pericarditis, and cardiomyopathy after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34340927/
- Clinical Guidance for Young People with Myocarditis and Pericarditis after Vaccination with COVID-19 mRNA: https://www.cps.ca/en/documents/position/clinical-guidance-for-youth-with-myocarditis-and-pericarditis
- Myocarditis / pericarditis associated with COVID-19 vaccine: https://science.gc.ca/eic/site/063.nsf/eng/h_98291.html
- Acute myocarditis after the second dose of SARS-CoV-2 vaccine: serendipity or causal relationship: https://pubmed.ncbi.nlm.nih.gov/34236331/
- Pericarditis after administration of COVID-19 mRNA BNT162b2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34364831/
- Unusual presentation of acute pericarditis after vaccination against SARS-COV-2 mRNA-1237 Modern: https://pubmed.ncbi.nlm.nih.gov/34447639/
- A case series of acute pericarditis after vaccination with COVID-19 in the context of recent reports from Europe and the United States: https://pubmed.ncbi.nlm.nih.gov/34635376/
- Acute pericarditis and cardiac tamponade after vaccination with Covid-19: https://pubmed.ncbi.nlm.nih.gov/34749492/
- Pericarditis after administration of the BNT162b2 mRNA vaccine COVID-19: https://pubmed.ncbi.nlm.nih.gov/34149145/
- Case report: symptomatic pericarditis post COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34693198/.
Μυοπερικαρδίτιδα
- Myopericarditis after Pfizer mRNA COVID-19 vaccination in adolescents: https://www.sciencedirect.com/science/article/pii/S002234762100665X
- Myopericarditis after vaccination with COVID-19 mRNA in adolescents 12 to 18 years of age: https://www.sciencedirect.com/science/article/pii/S0022347621007368
- Important information on myopericarditis after vaccination with Pfizer COVID-19 mRNA in adolescents: https://www.sciencedirect.com/science/article/pii/S0022347621007496
- Insights from a murine model of COVID-19 mRNA vaccine-induced myopericarditis: could accidental intravenous injection of a vaccine induce myopericarditis https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciab741/6359059
- Acute myocarditis after administration of BNT162b2 vaccine against COVID-19:.https://www.sciencedirect.com/science/article/abs/pii/S188558572100133X
- Insights from a murine model of myopericarditis induced by COVID-19 mRNA vaccine: could accidental intravenous injection of a vaccine induce myopericarditis: https://pubmed.ncbi.nlm.nih.gov/34453510/
- COVID-19 mRNA vaccination and development of CMR-confirmed myopericarditis: https://www.medrxiv.org/content/10.1101/2021.09.13.21262182v1.full?s=09.
- Intravenous injection of coronavirus disease 2019 (COVID-19) mRNA vaccine can induce acute myopericarditis in a mouse model: https://t.co/j0IEM8cMXI
- Myopericarditis in a previously healthy adolescent male after COVID-19 vaccination: Case report: https://pubmed.ncbi.nlm.nih.gov/34133825/
- Report of a case of myopericarditis after vaccination with BNT162b2 COVID-19 mRNA in a young Korean male: https://pubmed.ncbi.nlm.nih.gov/34636504/
- Myopericarditis after Pfizer messenger ribonucleic acid coronavirus coronavirus disease vaccine in adolescents: https://pubmed.ncbi.nlm.nih.gov/34228985/
- Acute myopericarditis after COVID-19 vaccine in adolescents: https://pubmed.ncbi.nlm.nih.gov/34589238/
- Nygaard, U., Holm, M., Bohnstedt, C., Chai, Q., Schmidt, L. S., Hartling, U. B., . . .Stensballe, L. G. (2022). Population-based Incidence of Myopericarditis After COVID-19 Vaccination in Danish Adolescents. Pediatr Infect Dis J, 41(1), e25-e28. doi:10.1097/INF.0000000000003389. https://www.ncbi.nlm.nih.gov/pubmed/34889875
- Schauer, J., Buddhe, S., Colyer, J., Sagiv, E., Law, Y., Mallenahalli Chikkabyrappa, S., & Portman, M. A. (2021). Myopericarditis After the Pfizer Messenger Ribonucleic Acid Coronavirus Disease Vaccine in Adolescents. J Pediatr, 238, 317-320. doi: 10.1016/j.jpeds.2021.06.083. https://www.ncbi.nlm.nih.gov/pubmed/34228985
- Kohli, U., Desai, L., Chowdhury, D., Harahsheh, A. S., Yonts, A. B., Ansong, A., . . .Ang, J. Y. (2021). mRNA Coronavirus-19 Vaccine-Associated Myopericarditis in Adolescents: A Survey Study. J Pediatr. doi:10.1016/j.jpeds.2021.12.025. https://www.ncbi.nlm.nih.gov/pubmed/34952008
- Long, S. S. (2021). Important Insights into Myopericarditis after the Pfizer mRNA COVID-19 Vaccination in Adolescents. J Pediatr, 238, 5. doi:10.1016/j.jpeds. 2021.07.057. https://www.ncbi.nlm.nih.gov/pubmed/34332972
- McLean, K., & Johnson, T. J. (2021). Myopericarditis in a previously healthy adolescent male following COVID-19 vaccination: A case report. Acad Emerg Med, 28(8), 918-921. doi:10.1111/acem.14322. https://www.ncbi.nlm.nih.gov/pubmed/34133825
- Umei, T. C., Kishino, Y., Shiraishi, Y., Inohara, T., Yuasa, S., & Fukuda, K. (2021). Recurrence of myopericarditis following mRNA COVID-19 vaccination in a male adolescent. CJC Open. doi:10.1016/j.cjco.2021.12.002. https://www.ncbi.nlm.nih.gov/pubmed/34904134
- Das, B. B., Kohli, U., Ramachandran, P., Nguyen, H. H., Greil, G., Hussain, T., . . .Khan, D. (2021). Myopericarditis after messenger RNA Coronavirus Disease 2019 Vaccination in Adolescents 12 to 18 Years of Age. J Pediatr, 238, 26-32 e21. doi: 10.1016/j.jpeds.2021.07.044. https://www.ncbi.nlm.nih.gov/pubmed/34339728
- Gatti, M., Raschi, E., Moretti, U., Ardizzoni, A., Poluzzi, E., & Diemberger, I. (2021). Influenza Vaccination and Myo-Pericarditis in Patients Receiving Immune Checkpoint Inhibitors: Investigating the Likelihood of Interaction through the Vaccine Adverse Event Reporting System and VigiBase. Vaccines (Basel), 9(1). doi:10.3390/vaccines9010019. https://www.ncbi.nlm.nih.gov/pubmed/33406694
- Myopericarditis in a previously healthy adolescent male after COVID-19 vaccination: Case report: https://pubmed.ncbi.nlm.nih.gov/34133825/
Περιμυοκαρδίτιδα
- Perimyocarditis in adolescents after Pfizer-BioNTech COVID-19 vaccine: https://academic.oup.com/jpids/advance-article/doi/10.1093/jpids/piab060/6329543
- Perimyocarditis in adolescents after Pfizer-BioNTech COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34319393/
- Unusual presentation of acute perimyocarditis after modern SARS-COV-2 mRNA-1237 vaccination: https://pubmed.ncbi.nlm.nih.gov/34447639/
- Perimyocarditis after the first dose of mRNA-1273 SARS-CoV-2 (Moderna) mRNA-1273 vaccine in a young healthy male: case report: https://bmccardiovascdisord.biomedcentral.com/articles/10.1186/s12872-021-02183
- Acute perimyocarditis after the first dose of COVID-19 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34515024/
- Perimyocarditis after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/
34866957/
- Tinoco, M., Leite, S., Faria, B., Cardoso, S., Von Hafe, P., Dias, G., . . . Lourenco, A. (2021). Perimyocarditis Following COVID-19 Vaccination. Clin Med Insights Cardiol, 15, 11795468211056634. doi:10.1177/11795468211056634. https://www.ncbi.nlm.nih.gov/pubmed/34866957
- Jhaveri, R., Adler-Shohet, F. C., Blyth, C. C., Chiotos, K., Gerber, J. S., Green, M., . . . Zaoutis, T. (2021). Weighing the Risks of Perimyocarditis With the Benefits of SARS-CoV-2 mRNA Vaccination in Adolescents. J Pediatric Infect Dis Soc, 10(10), 937-939. doi:10.1093/jpids/piab061. https://www.ncbi.nlm.nih.gov/pubmed/34270752
- Khogali, F., & Abdelrahman, R. (2021). Unusual Presentation of Acute Perimyocarditis Following SARS-COV-2 mRNA-1237 Moderna Vaccination. Cureus, 13(7), e16590. doi:10.7759/cureus.16590. https://www.ncbi.nlm.nih.gov/pubmed/34447639
- Hasnie, A. A., Hasnie, U. A., Patel, N., Aziz, M. U., Xie, M., Lloyd, S. G., & Prabhu, S. D. (2021). Perimyocarditis following first dose of the mRNA-1273 SARS-CoV-2 (Moderna) vaccine in a healthy young male: a case report. BMC Cardiovasc Disord, 21(1), 375. doi:10.1186/s12872-021-02183-3. https://www.ncbi.nlm.nih.gov/pubmed/34348657
Καρδιομυοπάθεια Tatsokubo
- Myocarditis, pericarditis and cardiomyopathy after COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S1443950621011562
- Takotsubo cardiomyopathy after vaccination with mRNA COVID-19: https://www.sciencedirect.com/science/article/pii/S1443950621011331
- Takotsubo (stress) cardiomyopathy after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34625447/
- Takotsubo cardiomyopathy after coronavirus 2019 vaccination in patient on maintenance hemodialysis: https://pubmed.ncbi.nlm.nih.gov/34731486/.
- Takotsubo syndrome after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34539938/.
Γενικές καρδιακές επιπλοκές
- Transient cardiac injury in adolescents receiving the BNT162b2 mRNA COVID-19 vaccine: https://journals.lww.com/pidj/Abstract/9000/Transient_Cardiac_Injury_in_Adolesce nts_Receiving.95800.aspx
- Snapiri, O., Rosenberg Danziger, C., Shirman, N., Weissbach, A., Lowenthal, A., Ayalon, I., . . . Bilavsky, E. (2021). Transient Cardiac Injury in Adolescents Receiving the BNT162b2 mRNA COVID-19 Vaccine. Pediatr Infect Dis J, 40(10), e360-e363. doi:10.1097/INF.0000000000003235. https://www.ncbi.nlm.nih.gov/pubmed/34077949
- Fazlollahi, A., Zahmatyar, M., Noori, M., Nejadghaderi, S. A., Sullman, M. J. M., Shekarriz-Foumani, R., . . . Safiri, S. (2021). Cardiac complications following mRNA COVID-19 vaccines: A systematic review of case reports and case series. Rev Med Virol, e2318. doi:10.1002/rmv.2318. https://www.ncbi.nlm.nih.gov/pubmed/34921468
- Ho, J. S., Sia, C. H., Ngiam, J. N., Loh, P. H., Chew, N. W., Kong, W. K., & Poh, K. K. (2021). A review of COVID-19 vaccination and the reported cardiac manifestations. Singapore Med J. doi:10.11622/smedj.2021210. https://www.ncbi.nlm.nih.gov/pubmed/34808708
- Temporal relationship between the second dose of BNT162b2 mRNA Covid-19 vaccine and cardiac involvement in a patient with previous SARS-COV-2 infection: https://www.sciencedirect.com/science/article/pii/S2352906721000622
- Cardiovascular, neurological, and pulmonary events after vaccination with BNT162b2, ChAdOx1 nCoV-19, and Ad26.COV2.S vaccines: an analysis of European data: https://pubmed.ncbi.nlm.nih.gov/34710832/
Οξύ στεφανιαίο σύνδρομο
- Mrna COVID vaccines dramatically increase endothelial inflammatory markers and risk of Acute Coronary Syndrome as measured by PULS cardiac testing: a caution: https://www.ahajournals.org/doi/10.1161/circ.144.suppl_1.10712
- Boivin Z. et al.Untimely Myocardial Infarction or COVID-19 Vaccine Side Effect. Cureus 13(3). B
Καρδιακό άλγος
See paper below
- Chest pain with abnormal electrocardiogram redevelopment after injection of COVID-19 vaccine manufactured by Moderna: https://pubmed.ncbi.nlm.nih.gov/34866106/
Σύνδρομο Κουνή (οξύ στεφανιαίο σύνδρομο λόγω αλλεργικής ή ανοσολογικής αντίδρασης)
- Kounis syndrome type 1 induced by inactivated SARS-COV-2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34148772/
- Kounis N. Kounis Syndrome—not a Single-organ Arterial Disorder but a Multisystem and multidisciplinary Disease. Balkan Med J 2019;36:212-21.
- Kounis N. et al.Kounis syndrome: a new twist on an old disease. Review. Future Cardiol. 2011 Nov;7(6):805-24.
- Boivin Z. et al.Untimely Myocardial Infarction or COVID-19 Vaccine Side Effect. Cureus 13(3). B
- Kounis N. et al., Allergic Reactions to Current Available COVID-19 Vaccinations: Pathophysiology, Causality, and Therapeutic Considerations. Vaccines 2021, 9,221.
ΘΡΟΜΒΩΣΕΙΣ
- Three cases of acute venous thromboembolism in women after vaccination against COVID-19: https://www.sciencedirect.com/science/article/pii/S2213333X21003929
- Acute thrombosis of the coronary tree after vaccination against COVID-19: https://www.sciencedirect.com/science/article/abs/pii/S1936879821003988
- US case reports of cerebral venous sinus thrombosis with thrombocytopenia after vaccination with Ad26.COV2.S (against covid-19), March 2 to April 21, 2020: https://pubmed.ncbi.nlm.nih.gov/33929487/
- Portal vein thrombosis associated with ChAdOx1 nCov-19 vaccine: https://www.thelancet.com/journals/langas/article/PIIS2468-1253(21)00197-7/
- Management of cerebral and splanchnic vein thrombosis associated with thrombocytopenia in subjects previously vaccinated with Vaxzevria (AstraZeneca): position statement of the Italian Society for the Study of Hemostasis and Thrombosis (SISET): https://pubmed.ncbi.nlm.nih.gov/33871350/
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 vaccines: https://www.sciencedirect.com/science/article/abs/pii/S0735675721004381
- Covid-19 vaccine-induced thrombosis and thrombocytopenia: a commentary on an important and practical clinical dilemma: https://www.sciencedirect.com/science/article/abs/pii/S0033062021000505
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 viral vector vaccines: https://www.sciencedirect.com/science/article/abs/pii/S0953620521001904
- COVID-19 vaccine-induced immune-immune thrombotic thrombocytopenia: an emerging cause of splanchnic vein thrombosis: https://www.sciencedirect.com/science/article/pii/S1665268121000557
- The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune thrombotic immune thrombocytopenia (covid): https://www.sciencedirect.com/science/article/pii/S1050173821000967
- Roots of autoimmunity of thrombotic events after COVID-19 vaccination: https://www.sciencedirect.com/science/article/abs/pii/S1568997221002160
- Thrombotic immune thrombocytopenia induced by SARS-CoV-2 vaccine: https://www.nejm.org/doi/full/10.1056/nejme2106315
- Thrombosis and thrombocytopenia after vaccination with ChAdOx1 nCoV-19: https://www.nejm.org/doi/full/10.1056/NEJMoa2104882?query=recirc_curatedRelated_article
- Thrombotic thrombocytopenia after vaccination with ChAdOx1 nCov-19: https://www.nejm.org/doi/full/10.1056/NEJMoa2104840?query=recirc_curatedRelated_article
- Post-mortem findings in vaccine-induced thrombotic thrombocytopenia (covid-19): https://haematologica.org/article/view/haematol.2021.279075
- Comparison of vaccine-induced thrombotic episodes between ChAdOx1 nCoV-19 and Ad26.COV.2.S vaccines: https://www.sciencedirect.com/science/article/abs/pii/S0896841121000895
- Hypothesis behind the very rare cases of thrombosis with thrombocytopenia syndrome after SARS-CoV-2 vaccination: https://www.sciencedirect.com/science/article/abs/pii/S0049384821003315
- Primary adrenal insufficiency associated with thrombotic immune thrombocytopenia induced by the Oxford-AstraZeneca ChAdOx1 nCoV-19 vaccine (VITT): https://www.sciencedirect.com/science/article/pii/S0953620521002363
- “Portal vein thrombosis occurring after the first dose of SARS-CoV-2 mRNA vaccine in a patient with antiphospholipid syndrome”: https://www.sciencedirect.com/science/article/pii/S2666572721000389
- Early results of bivalirudin treatment for thrombotic thrombocytopenia and cerebral venous sinus thrombosis after vaccination with Ad26.COV2.S: https://www.sciencedirect.com/science/article/pii/S0196064421003425
- Mechanisms of immunothrombosis in vaccine-induced thrombotic thrombocytopenia (VITT) compared to natural SARS-CoV-2 infection: https://www.sciencedirect.com/science/article/abs/pii/S0896841121000706
- Prothrombotic immune thrombocytopenia after COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S0006497121009411
- Vaccine-induced thrombotic thrombocytopenia: the dark chapter of a success story: https://www.sciencedirect.com/science/article/pii/S2589936821000256
- Thrombosis after COVID-19 vaccination: possible link to ACE pathways: https://www.sciencedirect.com/science/article/pii/S0049384821004369
- Vaccine-induced thrombotic thrombocytopenia, a rare but severe case of friendly fire in the battle against the COVID-19 pandemic: What pathogenesis?: https://www.sciencedirect.com/science/article/pii/S0953620521002314
- Thrombocytopenia and intracranial venous sinus thrombosis after exposure to the “AstraZeneca COVID-19 vaccine”: https://pubmed.ncbi.nlm.nih.gov/33918932/
- Thrombosis with thrombocytopenia after messenger RNA vaccine -1273: https://pubmed.ncbi.nlm.nih.gov/34181446/
- First dose of ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic, and hemorrhagic events in Scotland: https://www.nature.com/articles/s41591-021-01408-4
- PF4 immunoassays in vaccine-induced thrombotic thrombocytopenia: https://www.nejm.org/doi/full/10.1056/NEJMc2106383
- Antibody epitopes in vaccine-induced immune immune thrombotic thrombocytopenia: https://www.nature.com/articles/s41586-021-03744-4
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 vaccines:. https://www.sciencedirect.com/science/article/abs/pii/S0735675721004381.
- Immune thrombosis and thrombocytopenia (VITT) associated with the COVID-19 vaccine: diagnostic and therapeutic recommendations for a new syndrome: https://pubmed.ncbi.nlm.nih.gov/33987882/
- Laboratory testing for suspicion of COVID-19 vaccine-induced thrombotic (immune) thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34138513/
- Intracerebral haemorrhage due to thrombosis with thrombocytopenia syndrome after COVID-19 vaccination: the first fatal case in Korea: https://pubmed.ncbi.nlm.nih.gov/34402235/
- Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and positive SARS-CoV-2 tests: self-controlled case series study: https://pubmed.ncbi.nlm.nih.gov/34446426/
- Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis after covid-19 vaccination; a systematic review: https://pubmed.ncbi.nlm.nih.gov/34365148/.
- Primary adrenal insufficiency associated with thrombotic immune thrombocytopenia induced by Oxford-AstraZeneca ChAdOx1 nCoV-19 vaccine (VITT): https://pubmed.ncbi.nlm.nih.gov/34256983/
- Thromboaspiration infusion and fibrinolysis for portomesenteric thrombosis after administration of AstraZeneca COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34132839/
- 59-year-old woman with extensive deep venous thrombosis and pulmonary thromboembolism 7 days after a first dose of Pfizer-BioNTech BNT162b2 mRNA vaccine COVID-19: https://pubmed.ncbi.nlm.nih.gov/34117206/
- Thrombosis with thrombocytopenia syndrome (TTS) following AstraZeneca ChAdOx1 nCoV-19 (AZD1222) COVID-19 vaccination: risk-benefit analysis for persons <60 years in Australia: https://pubmed.ncbi.nlm.nih.gov/34272095/
- Comparison of vaccine-induced thrombotic events between ChAdOx1 nCoV-19 and Ad26.COV.2.S vaccines: https://pubmed.ncbi.nlm.nih.gov/34139631/.
- Bilateral superior ophthalmic vein thrombosis, ischemic stroke and immune thrombocytopenia after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/33864750/
- celiac artery and splenic artery thrombosis complicated by splenic infarction 7 days after the first dose of Oxford vaccine, causal relationship or coincidence: https://pubmed.ncbi.nlm.nih.gov/34261633/.
- Primary adrenal insufficiency associated with Oxford-AstraZeneca ChAdOx1 nCoV-19 (VITT) vaccine-induced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34256983/
- Thrombosis with thrombocytopenia syndrome after COVID-19 immunization: https://pubmed.ncbi.nlm.nih.gov/34236343/
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 viral vector vaccines: https://pubmed.ncbi.nlm.nih.gov/34092488/
- Thromboaspiration infusion and fibrinolysis for portomesenteric thrombosis after administration of the AstraZeneca COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34132839/.
- Atypical thrombosis associated with the vaccine VaxZevria® (AstraZeneca): data from the French network of regional pharmacovigilance centers: https://pubmed.ncbi.nlm.nih.gov/34083026/.
- Vaccine-induced thrombosis and thrombocytopenia with bilateral adrenal haemorrhage: https://pubmed.ncbi.nlm.nih.gov/34235757/.
- Palmar digital vein thrombosis after Oxford-AstraZeneca COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34473841/.
- Cutaneous thrombosis associated with cutaneous necrosis following Oxford- AstraZeneca COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34189756/
- Thrombosis with thrombocytopenia after Messenger vaccine RNA-1273: https://pubmed.ncbi.nlm.nih.gov/34181446/
- Coronavirus (COVID-19) Vaccine-induced immune thrombotic thrombocytopenia (VITT): https://pubmed.ncbi.nlm.nih.gov/34033367/
- Comparison of adverse drug reactions among four COVID-19 vaccines in Europe using the EudraVigilance database: Thrombosis in unusual sites: https://pubmed.ncbi.nlm.nih.gov/34375510/
- Immunoglobulin adjuvant for vaccine-induced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34107198/
- Severe vaccine-induced thrombotic thrombocytopenia following vaccination with COVID-19: an autopsy case report and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34355379/.
- Platelet activation and modulation in thrombosis with thrombocytopenia syndrome associated with the ChAdO Χ 1 nCov-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34474550/
- Report of the International Cerebral Venous Thrombosis Consortium on cerebral venous thrombosis after SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34462996/
- Immune thrombocytopenia associated with the Pfizer-BioNTech COVID-19 mRNA vaccine BNT162b2: https://www.sciencedirect.com/science/article/pii/S2214250921002018
- Secondary immune thrombocytopenia putatively attributable to COVID-19 vaccination: https://casereports.bmj.com/content/14/5/e242220.abstract.
- Immune thrombocytopenia following Pfizer-BioNTech BNT162b2 mRNA COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34155844/
- Newly diagnosed idiopathic thrombocytopenia after COVID-19 vaccine administration: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8176657/.
- Idiopathic thrombocytopenic purpura and the Moderna Covid-19 vaccine: https://www.annemergmed.com/article/S0196-0644(21)00122-0/fulltext.
- Thrombocytopenia after Pfizer and Moderna SARS vaccination – CoV -2: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8014568/.
- Immune thrombocytopenic purpura and acute liver injury after COVID-19 vaccination: https://casereports.bmj.com/content/14/7/e242678.
- Carotid artery immune thrombosis induced by adenovirus-vectored COVID-19 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34312301/.
- The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune-immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34455073/
- Cerebral venous sinus thrombosis negative for anti-PF4 antibody without thrombocytopenia after immunization with COVID-19 vaccine in a non-comorbid elderly Indian male treated with conventional heparin-warfarin-based anticoagulation: https://pubmed.ncbi.nlm.nih.gov/34186376/
- Arterial events, venous thromboembolism, thrombocytopenia and bleeding after vaccination with Oxford-AstraZeneca ChAdOx1-S in Denmark and Norway: population-based cohort study: https://pubmed.ncbi.nlm.nih.gov/33952445/
- Procoagulant microparticles: a possible link between vaccine-induced immune thrombocytopenia (VITT) and cerebral sinus venous thrombosis: https://pubmed.ncbi.nlm.nih.gov/34129181/
- U.S. case reports of cerebral venous sinus thrombosis with thrombocytopenia after vaccination with Ad26.COV2.S, March 2-April 21, 2021: https://pubmed.ncbi.nlm.nih.gov/33929487/.
- Malignant cerebral infarction after vaccination with ChAdOx1 nCov-19: a catastrophic variant of vaccine-induced immune-mediated thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34341358/
- Acute ischemic stroke revealing immune thrombotic thrombocytopenia induced by ChAdOx1 nCov-19 vaccine: impact on recanalization strategy: https://pubmed.ncbi.nlm.nih.gov/34175640/
- Vaccine-induced immune thrombotic immune thrombocytopenia (VITT): a new clinicopathologic entity with heterogeneous clinical presentations: https://pubmed.ncbi.nlm.nih.gov/34159588/.
- Imaging and hematologic findings in thrombosis and thrombocytopenia after vaccination with ChAdOx1 nCoV-19 (AstraZeneca): https://pubmed.ncbi.nlm.nih.gov/34402666/
- Autoimmunity roots of thrombotic events after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34508917/
- Cerebral venous sinus thrombosis after vaccination: the UK experience: https://pubmed.ncbi.nlm.nih.gov/34370974/
- Cutaneous thrombosis associated with cutaneous necrosis following Oxford-AstraZeneca COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34189756/
- Myocardial infarction and azygos vein thrombosis after vaccination with ChAdOx1 nCoV-19 in a hemodialysis patient: https://pubmed.ncbi.nlm.nih.gov/34650896/
- Refractory vaccine-induced immune thrombotic thrombocytopenia (VITT) treated with delayed therapeutic plasma exchange (TPE): https://pubmed.ncbi.nlm.nih.gov/
34672380/.
- Rare case of COVID-19 vaccine-associated intracranial hemorrhage with venous sinus thrombosis: https://pubmed.ncbi.nlm.nih.gov/34556531/.
- Delayed headache after COVID-19 vaccination: a warning sign for vaccine-induced cerebral venous thrombosis: https://pubmed.ncbi.nlm.nih.gov/34535076/.
- Clinical features of vaccine-induced thrombocytopenia and immune thrombosis: https://pubmed.ncbi.nlm.nih.gov/34379914/.
- Predictors of mortality in thrombotic thrombocytopenia after adenoviral COVID-19 vaccination: the FAPIC score: https://pubmed.ncbi.nlm.nih.gov/34545400/
- Ischemic stroke as a presenting feature of immune thrombotic thrombocytopenia induced by ChAdOx1-nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34035134/
- Endovascular treatment for vaccine-induced cerebral venous sinus thrombosis and thrombocytopenia after vaccination with ChAdOx1 nCoV-19: report of three cases: https://pubmed.ncbi.nlm.nih.gov/34782400/
- Possible triggers of thrombocytopenia and/or hemorrhage by BNT162b2 vaccine, Pfizer-BioNTech: https://pubmed.ncbi.nlm.nih.gov/34660652/.
- Multiple sites of arterial thrombosis in a 35-year-old patient after vaccination with ChAdOx1 (AstraZeneca), which required emergency femoral and carotid surgical thrombectomy: https://pubmed.ncbi.nlm.nih.gov/34644642/
- Case series of vaccine-induced thrombotic thrombocytopenia in a London teaching hospital: https://pubmed.ncbi.nlm.nih.gov/34694650/
- Neuro-ophthalmic complications with thrombocytopenia and thrombosis induced by ChAdOx1 nCoV-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34726934/
- Thrombotic events after COVID-19 vaccination in over 50 years of age: results of a population-based study in Italy: https://pubmed.ncbi.nlm.nih.gov/34835237/
- Intracerebral hemorrhage associated with vaccine-induced thrombotic thrombocytopenia after ChAdOx1 nCOVID-19 vaccination in a pregnant woman:
https://pubmed.ncbi.nlm.nih.gov/34261297/
- Age- and sex-specific incidence of cerebral venous sinus thrombosis associated with Ad26.COV2.S COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34724036/.
- Genital necrosis with cutaneous thrombosis following vaccination with COVID-19 mRNA: https://pubmed.ncbi.nlm.nih.gov/34839563/
- Cerebral venous sinus thrombosis after mRNA-based COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34783932/.
- COVID-19 vaccine-induced immune thrombosis with thrombocytopenia thrombosis (VITT) and shades of gray in thrombus formation: https://pubmed.ncbi.nlm.nih.gov/34624910/
- Acute ST-segment elevation myocardial infarction secondary to vaccine-induced immune thrombosis with thrombocytopenia (VITT): https://pubmed.ncbi.nlm.nih.gov/34580132/
- Thrombosis with thrombocytopenia syndrome (TTS) after vaccination with AstraZeneca ChAdOx1 nCoV-19 (AZD1222) COVID-19: a risk-benefit analysis for persons <60% risk-benefit analysis for people <60 years in Australia: https://pubmed.ncbi.nlm.nih.gov/34272095/
- Characteristics and outcomes of patients with cerebral venous sinus thrombosis in thrombotic immune thrombocytopenia induced by SARS-CoV-2 vaccine: https://jamanetwork.com/journals/jamaneurology/fullarticle/2784622
100.Case study of thrombosis and thrombocytopenia syndrome after administration of the AstraZeneca COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34781321/
101.Thrombosis with Thrombocytopenia Syndrome Associated with COVID-19 Vaccines: https://pubmed.ncbi.nlm.nih.gov/34062319/
102.Cerebral venous sinus thrombosis following vaccination with ChAdOx1: the first case of definite thrombosis with thrombocytopenia syndrome in India: https://pubmed.ncbi.nlm.nih.gov/34706921/
103.COVID-19 vaccine-associated thrombosis with thrombocytopenia syndrome (TTS): systematic review and post hoc analysis: https://pubmed.ncbi.nlm.nih.gov/34698582/
104.Concerns for adverse effects of thrombocytopenia and thrombosis after adenovirusvectored COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34541935/
105.Cerebral venous sinus thrombosis after COVID-19 vaccination: neurologic and radiologic management: https://pubmed.ncbi.nlm.nih.gov/34327553/.
106.Case report: cerebral sinus vein thrombosis in two patients with AstraZeneca SARSCoV-2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34609603/
107.Vaccine-induced immune thrombosis and thrombocytopenia syndrome after adenovirus-vectored severe acute respiratory syndrome coronavirus 2 vaccination: a new hypothesis on mechanisms and implications for future vaccine development: https://pubmed.ncbi.nlm.nih.gov/34664303/.
108.Thrombosis in peripheral artery disease and thrombotic thrombocytopenia following adenoviral COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34649281/
109.Cerebral venous sinus thrombosis and thrombotic events after vector-based COVID-19 vaccines: systematic review and meta-analysis: https://pubmed.ncbi.nlm.nih.gov/34610990/.
110.Thrombosis after COVID-19 vaccination: possible link to ACE pathways: https://pubmed.ncbi.nlm.nih.gov/34479129/
111.Major artery thrombosis and vaccination against ChAdOx1 nCov-19: https://pubmed.ncbi.nlm.nih.gov/34839830/
112.Understanding the risk of thrombosis with thrombocytopenia syndrome followingAd26.COV2.S vaccination: https://pubmed.ncbi.nlm.nih.gov/34595694/
113.Comments on thrombosis after vaccination: spike protein leader sequence could be responsible for thrombosis and antibody-mediated thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34788138
114.Thrombosis in pre- and post-vaccination phase of COVID-19; https://pubmed.ncbi.nlm.nih.gov/34650382/
115.Vaccine-associated thrombocytopenia and thrombosis: venous endotheliopathy leading to combined venous micro-macrothrombosis: https://pubmed.ncbi.nlm.nih.gov/34833382/
116.Thrombosis and thrombocytopenia syndrome causing isolated symptomatic carotid occlusion after COVID-19 Ad26.COV2.S vaccine (Janssen): https://pubmed.ncbi.nlm.nih.gov/34670287/
117.An unusual presentation of acute deep vein thrombosis after Moderna COVID-19 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34790811/
118.Immediate high-dose intravenous immunoglobulins followed by direct treatment with thrombin inhibitors is crucial for survival in vaccine-induced immune thrombotic thrombocytopenia Sars-Covid-19-vector adenoviral VITT with venous thrombosis of the cerebral sinus and portal vein: https://pubmed.ncbi.nlm.nih.gov/34023956/.
119.Thrombosis formation after COVID-19 vaccination immunologic aspects: review article: https://pubmed.ncbi.nlm.nih.gov/34629931/
120.Imaging and hematologic findings in thrombosis and thrombocytopenia after vaccination with ChAdOx1 nCoV-19 (AstraZeneca): https://pubmed.ncbi.nlm.nih.gov/ 34402666/
121.Cerebral venous sinus thrombosis, pulmonary embolism, and thrombocytopenia after COVID-19 vaccination in a Taiwanese man: a case report and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34630307/
122.Fatal cerebral venous sinus thrombosis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33983464/
123.Autoimmune roots of thrombotic events after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34508917/.
124.New portal vein thrombosis in cirrhosis: is thrombophilia exacerbated by vaccine or COVID-19: https://www.jcehepatology.com/article/S0973-6883(21)00545-4/fulltext.
125.Cerebral venous sinus thrombosis after vaccination with COVID-19 mRNA of BNT162b2: https://pubmed.ncbi.nlm.nih.gov/34796065/.
126.A case of unusual mild clinical presentation of COVID-19 vaccine-induced immune thrombotic thrombocytopenia with splanchnic vein thrombosis: https://pubmed.ncbi.nlm.nih.gov/34843991/
127.Cerebral venous sinus thrombosis following vaccination with Pfizer-BioNTech COVID-19 (BNT162b2): https://pubmed.ncbi.nlm.nih.gov/34595867/
128.A case of idiopathic thrombocytopenic purpura after a booster dose of COVID-19 BNT162b2 vaccine (Pfizer-Biontech): https://pubmed.ncbi.nlm.nih.gov/34820240/
- Vaccine-induced immune thrombotic immune thrombocytopenia (VITT): targeting
pathologic mechanisms with Bruton’s tyrosine kinase inhibitors: https://pubmed.ncbi.nlm.nih.gov/33851389/
130.Thromboembolic events in younger females exposed to Pfizer-BioNTech or Moderna COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34264151/
131.Thrombosis after adenovirus-vectored COVID-19 vaccination: a concern for underlying disease: https://pubmed.ncbi.nlm.nih.gov/34755555/
132.Unusual site of deep vein thrombosis after vaccination against coronavirus mRNA-2019 coronavirus disease (COVID-19): https://pubmed.ncbi.nlm.nih.gov/34840204/
133.Deep venous thrombosis after vaccination with Ad26.COV2.S in adult males: https://pubmed.ncbi.nlm.nih.gov/34659839/.
134.Clinical and biological features of cerebral venous sinus thrombosis after vaccination with ChAdOx1 nCov-19; https://jnnp.bmj.com/content/early/2021/09/29/jnnp-2021-327340.
135.CAd26.COV2-S vaccination may reveal hereditary thrombophilia: massive cerebral venous sinus thrombosis in a young man with normal platelet count: https://pubmed.ncbi.nlm.nih.gov/34632750/
136.Post-mortem findings in vaccine-induced thrombotic thrombocytopenia: https://haematologica.org/article/view/haematol.2021.279075
137.COVID-19 vaccine-induced thrombosis: https://pubmed.ncbi.nlm.nih.gov/34802488/.
138.Inflammation and platelet activation after COVID-19 vaccines: possible mechanisms behind vaccine-induced immune thrombocytopenia and thrombosis: https://pubmed.ncbi.nlm.nih.gov/34887867/.
139.Anaphylactoid reaction and coronary thrombosis related to COVID-19 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34863404/.
140.Occurrence of splenic infarction due to arterial thrombosis after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34876440/
141.Deep venous thrombosis more than two weeks after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33928773/
142.Information on ChAdOx1 nCoV-19 vaccine-induced immune-mediated thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34587242/
143.Management of a patient with a rare congenital limb malformation syndrome after SARS-CoV-2 vaccine-induced thrombosis and thrombocytopenia (VITT): https://pubmed.ncbi.nlm.nih.gov/34097311/
144.Thrombocytopenia and splanchnic thrombosis after vaccination with Ad26.COV2.S successfully treated with transjugular intrahepatic intrahepatic portosystemic shunt and thrombectomy: https://onlinelibrary.wiley.com/doi/10.1002/ajh.26258
145.Chang, J. C., & Hawley, H. B. (2021). Vaccine-Associated Thrombocytopenia and Thrombosis: Venous Endotheliopathy Leading to Venous Combined Micro-Macrothrombosis. Medicina (Kaunas), 57(11). doi:10.3390/medicina57111163. https://www.ncbi.nlm.nih.gov/pubmed/34833382
146.Potential risk of thrombotic events after COVID-19 vaccination with Oxford-AstraZeneca in women receiving estrogen: https://pubmed.ncbi.nlm.nih.gov/34734086/
147.Thrombotic adverse events reported for Moderna, Pfizer, and Oxford-AstraZeneca COVID-19 vaccines: comparison of occurrence and clinical outcomes in the EudraVigilance database: https://pubmed.ncbi.nlm.nih.gov/34835256/
148.Predicted and observed incidence of thromboembolic events among Koreans vaccinated with the ChAdOx1 nCoV-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34254476/
149.Three cases of acute venous thromboembolism in women after coronavirus 2019 vaccination: https://pubmed.ncbi.nlm.nih.gov/34352418/
150.Shazley, O., & Alshazley, M. (2021). A COVID-Positive 52-Year-Old Man Presented With Venous Thromboembolism and Disseminated Intravascular Coagulation Following Johnson & Johnson Vaccination: A Case-Study. Cureus, 13(7), e16383. doi:10.7759/cureus.16383. https://www.ncbi.nlm.nih.gov/pubmed/34408937
- Coagulopathies after SARS-CoV-2 vaccination may derive from a combined effect of SARS-CoV-2 spike protein and adenovirus vector-activated signaling pathways: https://pubmed.ncbi.nlm.nih.gov/34639132/
- Diffuse prothrombotic syndrome after administration of ChAdOx1 nCoV-19 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34615534/
- Calcaterra, G., Bassareo, P. P., Barilla, F., Romeo, F., & Mehta, J. L. (2022). Concerning the unexpected prothrombotic state following some coronavirus disease 2019 vaccines. J Cardiovasc Med (Hagerstown), 23(2), 71-74. doi:10.2459/JCM. 0000000000001232. https://www.ncbi.nlm.nih.gov/pubmed/34366403
- Blood clots and bleeding after BNT162b2 and ChAdOx1 nCoV-19 vaccination: an analysis of European data: https://pubmed.ncbi.nlm.nih.gov/34174723/
- Antiphospholipid antibodies and risk of thrombophilia after COVID-19 vaccination: the straw that breaks the camel’s back?: https://docs.google.com/document/d/1XzajasO8VMMnC3CdxSBKks1o7kiOLXFQ
Επεισόδια αυτοάνοσης θρομβωτικής θρομβοκυτοπενικής πορφύρας
- First report of a de novo iTTP episode associated with a COVID-19 mRNA-based anti-COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34105244/
Πνευμονική εμβολή
- Isolated pulmonary embolism after COVID vaccination: 2 case reports and a review of acute pulmonary embolism complications and follow-up: https://pubmed.ncbi.nlm.nih.gov/34804412/
- Myocardial infarction, stroke, and pulmonary embolism after BNT162b2 mRNA COVID-19 vaccine in persons aged 75 years or older: https://pubmed.ncbi.nlm.nih.gov/34807248/
- Pulmonary embolism, transient ischemic attack, and thrombocytopenia after Johnson & Johnson COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34261635/
- A case of acute pulmonary embolism after immunization with SARS-CoV-2 mRNA: https://pubmed.ncbi.nlm.nih.gov/34452028/
Θρόμβωση εγκεφαλικών φλεβωδών κόλπων
- Cerebral venous sinus thrombosis in the U.S. population after SARS-CoV-2 vaccination with adenovirus and after COVID-19: https://www.sciencedirect.com/science/article/pii/S0735109721051949
- Cerebral venous sinus thrombosis negative for anti-PF4 antibody without thrombocytopenia after immunization with COVID-19 vaccine in a non-comorbid elderly Indian male treated with conventional heparin-warfarin based anticoagulation: https://www.sciencedirect.com/science/article/pii/S1871402121002046
- Cerebral venous thrombosis after BNT162b2 mRNA SARS-CoV-2 vaccine: https://www.sciencedirect.com/science/article/abs/pii/S1052305721003098
- Cerebral venous sinus thrombosis after vaccination: the United Kingdom experience: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01788-8/fulltext
- US case reports of cerebral venous sinus thrombosis with thrombocytopenia after vaccination with Ad26.COV2.S (against covid-19), March 2 to April 21, 2020: https://pubmed.ncbi.nlm.nih.gov/33929487/
- Management of cerebral and splanchnic vein thrombosis associated with thrombocytopenia in subjects previously vaccinated with Vaxzevria (AstraZeneca): position statement of the Italian Society for the Study of Hemostasis and Thrombosis (SISET): https://pubmed.ncbi.nlm.nih.gov/33871350/
- Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis after vaccination with COVID-19; a systematic review: https://www.sciencedirect.com/science/article/pii/S0022510X21003014
- Early results of bivalirudin treatment for thrombotic thrombocytopenia and cerebral venous sinus thrombosis after vaccination with Ad26.COV2.S: https://www.sciencedirect.com/science/article/pii/S0196064421003425
- A rare case of a middle-aged Asian male with cerebral venous thrombosis after AstraZeneca COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S0735675721005714
- Cerebral venous sinus thrombosis and thrombocytopenia after COVID-19 vaccination: report of two cases in the United Kingdom: https://www.sciencedirect.com/science/article/abs/pii/S088915912100163X
- Diagnostic-therapeutic recommendations of the ad-hoc FACME expert working group on the management of cerebral venous thrombosis related to COVID-19 vaccination: https://www.sciencedirect.com/science/article/pii/S0213485321000839
- COVID-19 vaccination: information on the occurrence of arterial and venous thrombosis using data from VigiBase: https://pubmed.ncbi.nlm.nih.gov/33863748/
- Cerebral venous thrombosis associated with the covid-19 vaccine in Germany: https://onlinelibrary.wiley.com/doi/10.1002/ana.26172
- Cerebral venous thrombosis following BNT162b2 mRNA vaccination of BNT162b2 against SARS-CoV-2: a black swan event: https://pubmed.ncbi.nlm.nih.gov/34133027/
- The importance of recognizing cerebral venous thrombosis following anti-COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34001390/
- Cerebral venous sinus thrombosis negative for anti-PF4 antibody without thrombocytopenia after immunization with COVID-19 vaccine in an elderly, noncomorbid Indian male treated with conventional heparin-warfarin-based
anticoagulation:. https://www.sciencedirect.com/science/article/pii/S1871402121002046.
- Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis after covid-19 vaccination; a systematic review: https://pubmed.ncbi.nlm.nih.gov/34365148/.
- A rare case of cerebral venous thrombosis and disseminated intravascular coagulation temporally associated with administration of COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33917902/
- Acute cerebral venous thrombosis and pulmonary artery embolism associated with the COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34247246/.
- Cerebral venous thrombosis and vaccine-induced thrombocytopenia.a. Oxford-AstraZeneca COVID-19: a missed opportunity for a rapid return on experience: https://pubmed.ncbi.nlm.nih.gov/34033927/
- Diagnosis and treatment of cerebral venous sinus thrombosis with vaccine-induced immune-immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/33914590/
- Venous sinus thrombosis after vaccination with ChAdOx1 nCov-19: https://pubmed.ncbi.nlm.nih.gov/34420802/
- Cerebral venous sinus thrombosis following vaccination against SARS-CoV-2: an analysis of cases reported to the European Medicines Agency: https://pubmed.ncbi.nlm.nih.gov/34293217/
- Arterial events, venous thromboembolism, thrombocytopenia and bleeding after vaccination with Oxford-AstraZeneca ChAdOx1-S in Denmark and Norway: population-based cohort study: https://pubmed.ncbi.nlm.nih.gov/33952445/
- Cerebral venous thrombosis associated with COVID-19 vaccine in Germany: https://pubmed.ncbi.nlm.nih.gov/34288044/
- Malignant cerebral infarction after vaccination with ChAdOx1 nCov-19: a catastrophic variant of vaccine-induced immune-mediated thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34341358/
- Cerebral venous sinus thrombosis associated with thrombocytopenia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33845870/.
- central venous sinus thrombosis with subarachnoid hemorrhage after COVID-19 mRNA vaccination: are these reports merely coincidental: https://pubmed.ncbi.nlm.nih.gov/34478433/
- Cerebral venous sinus thrombosis negative for anti-PF4 antibody without thrombocytopenia after immunization with COVID-19 vaccine in a non-comorbid elderly Indian male treated with conventional heparin-warfarin-based anticoagulation: https://pubmed.ncbi.nlm.nih.gov/34186376/
- Cerebral venous sinus thrombosis 2 weeks after first dose of SARS-CoV-2 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34101024/
- Deep venous thrombosis (DVT) occurring shortly after second dose of SARS-CoV-2 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/33687691/
- Vaccine-induced immune thrombotic thrombocytopenia causing a severe form of cerebral venous thrombosis with high mortality rate: a case series: https://pubmed.ncbi.nlm.nih.gov/34393988/.
- Procoagulant microparticles: a possible link between vaccine-induced immune
thrombocytopenia (VITT) and cerebral sinus venous thrombosis: https://pubmed.ncbi.nlm.nih.gov/34129181/.
- Acute cerebral venous thrombosis and pulmonary artery embolism associated with the COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34247246/.
- Cerebral venous thrombosis following COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34045111/.
- Adverse effects reported after COVID-19 vaccination in a tertiary care hospital, centered on cerebral venous sinus thrombosis (CVST): https://pubmed.ncbi.nlm.nih.gov/34092166/
- Cerebral venous thrombosis associated with COVID-19 vaccine in Germany: https://pubmed.ncbi.nlm.nih.gov/34288044/.
- Cerebral venous sinus thrombosis after COVID-19 vaccination : Neurological and radiological management: https://pubmed.ncbi.nlm.nih.gov/34327553/.
- Cerebral venous thrombosis and thrombocytopenia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33878469/.
- Cerebral venous sinus thrombosis and thrombocytopenia after COVID-19 vaccination: report of two cases in the United Kingdom: https://pubmed.ncbi.nlm.nih.gov/33857630/.
- Cerebral venous thrombosis induced by SARS-CoV-2 vaccine: https:// pubmed.ncbi.nlm.nih.gov/34090750/.
- Cerebral venous sinus thrombosis associated with vaccine-induced thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34333995/
- Cerebral venous thrombosis after the BNT162b2 mRNA SARS-CoV-2 vaccine:
https://pubmed.ncbi.nlm.nih.gov/34111775/.
- Cerebral venous thrombosis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34045111/
- Lethal cerebral venous sinus thrombosis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33983464/
- Cerebral venous sinus thrombosis in the U.S. population, After SARS-CoV-2 vaccination with adenovirus and after COVID-19: https://pubmed.ncbi.nlm.nih.gov/34116145/
- Cerebral venous thrombosis after COVID-19 vaccination: is the risk of thrombosis increased by intravascular administration of the vaccine: https://pubmed.ncbi.nlm.nih.gov/34286453/.
- Central venous sinus thrombosis with subarachnoid hemorrhage after COVID-19 mRNA vaccination: are these reports merely coincidental: https://pubmed.ncbi.nlm.nih.gov/34478433/
- Cerebral venous sinus thrombosis after ChAdOx1 nCov-19 vaccination with a misleading first brain MRI: https://pubmed.ncbi.nlm.nih.gov/34244448/
- Early results of bivalirudin treatment for thrombotic thrombocytopenia and cerebral venous sinus thrombosis after vaccination with Ad26.COV2.S: https://pubmed.ncbi.nlm.nih.gov/34226070/
- Cerebral venous sinus thrombosis associated with post-vaccination thrombocytopenia by COVID-19: https://pubmed.ncbi.nlm.nih.gov/33845870/.
- Cerebral venous sinus thrombosis 2 weeks after the first dose of SARS-CoV-2 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34101024/.
- Adverse effects reported after COVID-19 vaccination in a tertiary care hospital, focus on cerebral venous sinus thrombosis (CVST): https://pubmed.ncbi.nlm.nih.gov/34092166/
- Cerebral venous sinus thrombosis following vaccination against SARS-CoV-2: an analysis of cases reported to the European Medicines Agency: https://pubmed.ncbi.nlm.nih.gov/34293217/
- A rare case of a middle-age Asian male with cerebral venous thrombosis after COVID-19 AstraZeneca vaccination: https://pubmed.ncbi.nlm.nih.gov/34274191/
- Massive cerebral venous thrombosis and venous basin infarction as late complications of COVID-19: a case report: https://pubmed.ncbi.nlm.nih.gov/34373991/
- Massive cerebral venous thrombosis due to vaccine-induced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34261296/
- Cerebral venous thrombosis developing after vaccination. COVID-19: VITT, VATT, TTS and more: https://pubmed.ncbi.nlm.nih.gov/34695859/
- Cerebral venous thrombosis and myeloproliferative neoplasms: a three-center study of 74 consecutive cases: https://pubmed.ncbi.nlm.nih.gov/34453762/.
- Vaccine-induced cerebral venous thrombosis and thrombocytopenia. Oxford-AstraZeneca COVID-19: a missed opportunity for rapid return on experience: https://www.sciencedirect.com/science/article/pii/S235255682100093X
- Case report: Take a second look: Cerebral venous thrombosis related to Covid-19 vaccination and thrombotic thrombocytopenia syndrome: https://pubmed.ncbi.nlm.nih.gov/34880826/
- Wittstock M, Walter U, Volmer E, Storch A, Weber MA, Großmann A. Cerebral venous sinus thrombosis after adenovirus-vectored COVID-19 vaccination: review of the neurological-neuroradiological procedure. Neuroradiology. 2022:1-10.
Θρομβωτική θρομβοκυτοπενική πορφύρα
- Thrombotic thrombocytopenic purpura after vaccination with Ad26.COV2-S: https://pubmed.ncbi.nlm.nih.gov/33980419/
- Thrombotic thrombocytopenic purpura: a new threat after COVID bnt162b2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34264514/.
- Severe immune thrombocytopenic purpura after SARS-CoV-2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34754937/
- Immune thrombocytopenic purpura associated with COVID-19 mRNA vaccine Pfizer-BioNTech BNT16B2b2: https://pubmed.ncbi.nlm.nih.gov/34077572/
Υπερπηκτικότητα
- COVID-19 vaccine in patients with hypercoagulability disorders: a clinical perspective: https://pubmed.ncbi.nlm.nih.gov/34786893/
Θρομβοφλεβίτιδα
- Idiopathic external jugular vein thrombophlebitis after coronavirus disease vaccination (COVID-19): https://pubmed.ncbi.nlm.nih.gov/33624509/.
ΘΡΟΜΒΟΠΕΝΙΑ
- Vaccine-induced immune thrombotic thrombocytopenia with disseminated intravascular coagulation and death after ChAdOx1 nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34171649/
- US case reports of cerebral venous sinus thrombosis with thrombocytopenia after vaccination with Ad26.COV2.S (against covid-19), March 2 to April 21, 2020: https://pubmed.ncbi.nlm.nih.gov/33929487/
- Management of cerebral and splanchnic vein thrombosis associated with thrombocytopenia in subjects previously vaccinated with Vaxzevria (AstraZeneca): position statement of the Italian Society for the Study of Hemostasis and Thrombosis (SISET): https://pubmed.ncbi.nlm.nih.gov/33871350/
- Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis after vaccination with COVID-19; a systematic review: https://www.sciencedirect.com/science/article/pii/S0022510X21003014
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 vaccines: https://www.sciencedirect.com/science/article/abs/pii/S0735675721004381
- Covid-19 vaccine-induced thrombosis and thrombocytopenia: a commentary on an important and practical clinical dilemma: https://www.sciencedirect.com/science/article/abs/pii/S0033062021000505
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 viral vector vaccines: https://www.sciencedirect.com/science/article/abs/pii/S0953620521001904
- COVID-19 vaccine-induced immune-immune thrombotic thrombocytopenia: an emerging cause of splanchnic vein thrombosis: https://www.sciencedirect.com/science/article/pii/S1665268121000557
- The roles of platelets in COVID-19-associated coagulopathy and vaccine-induced immune thrombotic immune thrombocytopenia (covid): https://www.sciencedirect.com/science/article/pii/S1050173821000967
- Thrombotic immune thrombocytopenia induced by SARS-CoV-2 vaccine: https://www.nejm.org/doi/full/10.1056/nejme2106315
- Thrombosis and thrombocytopenia after vaccination with ChAdOx1 nCoV-19: https://www.nejm.org/doi/full/10.1056/NEJMoa2104882?query=recirc_curatedRelated_article
- Post-mortem findings in vaccine-induced thrombotic thrombocytopenia (covid-19): https://haematologica.org/article/view/haematol.2021.279075
- Thrombocytopenia, including immune thrombocytopenia after receiving COVID-19 mRNA vaccines reported to the Vaccine Adverse Event Reporting System (VAERS): https://www.sciencedirect.com/science/article/pii/S0264410X21005247
- Hypothesis behind the very rare cases of thrombosis with thrombocytopenia syndrome after SARS-CoV-2 vaccination: https://www.sciencedirect.com/science/article/abs/pii/S0049384821003315
- Primary adrenal insufficiency associated with thrombotic immune thrombocytopenia induced by the Oxford-AstraZeneca ChAdOx1 nCoV-19 vaccine (VITT): https://www.sciencedirect.com/science/article/pii/S0953620521002363
- Early results of bivalirudin treatment for thrombotic thrombocytopenia and cerebral venous sinus thrombosis after vaccination with Ad26.COV2.S: https://www.sciencedirect.com/science/article/pii/S0196064421003425
- Mechanisms of immunothrombosis in vaccine-induced thrombotic thrombocytopenia (VITT) compared to natural SARS-CoV-2 infection: https://www.sciencedirect.com/science/article/abs/pii/S0896841121000706
- Vaccine-induced thrombotic thrombocytopenia: the dark chapter of a success story: https://www.sciencedirect.com/science/article/pii/S2589936821000256
- Cerebral venous sinus thrombosis and thrombocytopenia after COVID-19 vaccination: report of two cases in the United Kingdom: https://www.sciencedirect.com/science/article/abs/pii/S088915912100163X
- Immune thrombocytopenic purpura after vaccination with COVID-19 vaccine (ChAdOx1 nCov-19): https://www.sciencedirect.com/science/article/abs/pii/S0006497121013963.
- Vaccine-induced thrombotic thrombocytopenia, a rare but severe case of friendly fire in the battle against the COVID-19 pandemic: What pathogenesis?: https://www.sciencedirect.com/science/article/pii/S0953620521002314
- Thrombocytopenia and intracranial venous sinus thrombosis after exposure to the “AstraZeneca COVID-19 vaccine”: https://pubmed.ncbi.nlm.nih.gov/33918932/
- Thrombocytopenia following Pfizer and Moderna SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/33606296/
- Severe and refractory immune thrombocytopenia occurring after SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/33854395/
- Purpuric rash and thrombocytopenia after mRNA-1273 (Modern) COVID-19 vaccine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7996471/
- Thrombosis with thrombocytopenia after messenger RNA vaccine -1273: https://pubmed.ncbi.nlm.nih.gov/34181446/
- First dose of ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic, and hemorrhagic events in Scotland: https://www.nature.com/articles/s41591-021-01408-4
- Exacerbation of immune thrombocytopenia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34075578/
- PF4 immunoassays in vaccine-induced thrombotic thrombocytopenia: https://www.nejm.org/doi/full/10.1056/NEJMc2106383
- Antibody epitopes in vaccine-induced immune immune thrombotic thrombocytopenia: https://www.nature.com/articles/s41586-021-03744-4
- Thrombosis with thrombocytopenia syndrome associated with COVID-19 vaccines: https://www.sciencedirect.com/science/article/abs/pii/S0735675721004381.
- Immune thrombocytopenia associated with Pfizer-BioNTech’s COVID-19 BNT162b2 mRNA vaccine: https://www.sciencedirect.com/science/article/pii/S2214250921002018.
- Immune thrombosis and thrombocytopenia (VITT) associated with the COVID-19 vaccine: diagnostic and therapeutic recommendations for a new syndrome: https://pubmed.ncbi.nlm.nih.gov/33987882/
- Laboratory testing for suspicion of COVID-19 vaccine-induced thrombotic (immune) thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34138513/
- Intracerebral haemorrhage due to thrombosis with thrombocytopenia syndrome after COVID-19 vaccination: the first fatal case in Korea: https://pubmed.ncbi.nlm.nih.gov/34402235/
- Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and positive SARS-CoV-2 tests: self-controlled case series study: https://pubmed.ncbi.nlm.nih.gov/34446426/
- Vaccine-induced immune thrombotic thrombocytopenia and cerebral venous sinus thrombosis after covid-19 vaccination; a systematic review: https://pubmed.ncbi.nlm.nih.gov/34365148/.
- Primary adrenal insufficiency associated with thrombotic immune thrombocytopenia induced by Oxford-AstraZeneca ChAdOx1 nCoV-19 vaccine (VITT): https://pubmed.ncbi.nlm.nih.gov/34256983/
- Cerebral venous thrombosis and vaccine-induced thrombocytopenia.a. Oxford-AstraZeneca COVID-19: a missed opportunity for a rapid return on experience: https://pubmed.ncbi.nlm.nih.gov/34033927/
- Immune thrombocytopenia in a 22-year-old post Covid-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33476455/
- Secondary immune thrombocytopenia (ITP) associated with ChAdOx1 Covid-19 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34377889/
- Thrombosis with thrombocytopenia syndrome (TTS) following AstraZeneca ChAdOx1 nCoV-19 (AZD1222) COVID-19 vaccination: risk-benefit analysis for persons <60 years in Australia: https://pubmed.ncbi.nlm.nih.gov/34272095/
- Bilateral superior ophthalmic vein thrombosis, ischemic stroke and immune thrombocytopenia after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/33864750/
- Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and positive SARS-CoV-2 tests: self-controlled case series study: https://pubmed.ncbi.nlm.nih.gov/34446426/
- First dose of ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic and hemorrhagic events in Scotland: https://pubmed.ncbi.nlm.nih.gov/34108714/
- Thrombocytopenia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34332437/.
- A case of multiple thrombocytopenia and thrombosis following vaccination with ChAdOx1 nCoV-19 against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/34137813/
- Vaccine-induced thrombotic thrombocytopenia: the elusive link between thrombosis and adenovirus-based SARS-CoV-2 vaccines: https://pubmed.ncbi.nlm.nih.gov/34191218/
- Acute ischemic stroke revealing immune thrombotic thrombocytopenia induced by ChAdOx1 nCov-19 vaccine: impact on recanalization strategy: https://pubmed.ncbi.nlm.nih.gov/34175640/
- Procoagulant antibody-mediated procoagulant platelets in immune thrombotic thrombocytopenia associated with SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34011137/.
- Thrombotic thrombocytopenia after vaccination with COVID-19: in search of the underlying mechanism: https://pubmed.ncbi.nlm.nih.gov/34071883/
- Thrombosis and SARS-CoV-2 vaccines: vaccine-induced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34237213/.
- Acquired thrombotic thrombocytopenic thrombocytopenic purpura: a rare disease associated with the BNT162b2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34105247/.
- Immune complexes, innate immunity and NETosis in ChAdOx1 vaccine-induced thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34405870/.
- Immune-mediated thrombocytopenic purpura after Pfizer-BioNTech COVID-19 vaccine in an elderly woman: https://pubmed.ncbi.nlm.nih.gov/34513446/
- Immune-mediated thrombocytopenia associated with Ad26.COV2.S vaccine (Janssen; Johnson & Johnson): https://pubmed.ncbi.nlm.nih.gov/34469919/.
- Transient thrombocytopenia with glycoprotein-specific platelet autoantibodies after vaccination with Ad26.COV2.S: case report: https://pubmed.ncbi.nlm.nih.gov/34516272/.
- COVID-19 vaccine, immune thrombotic thrombocytopenia, jaundice, hyperviscosity: concern in cases with underlying hepatic problems: https://pubmed.ncbi.nlm.nih.gov/34509271/.
- Immune thrombocytopenia after vaccination during the COVID-19 pandemic: https://pubmed.ncbi.nlm.nih.gov/34435486/
- Vaccine-induced thrombocytopenia with severe headache: https://pubmed.ncbi.nlm.nih.gov/34525282/
- Vaccine-induced immune thrombotic thrombocytopenia causing a severe form of cerebral venous thrombosis with a high mortality rate: a case series: https://pubmed.ncbi.nlm.nih.gov/34393988/.
- Adenovirus interactions with platelets and coagulation and vaccine-associated autoimmune thrombocytopenia thrombosis syndrome: https://pubmed.ncbi.nlm.nih.gov/34407607/.
- Australian and New Zealand approach to the diagnosis and treatment of vaccineinduced immune thrombosis and immune thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34490632/
- An observational study to identify the prevalence of thrombocytopenia and anti-PF4 / polyanion antibodies in Norwegian health care workers after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33909350/
- A rare case of thrombosis and thrombocytopenia of the superior ophthalmic vein after
ChAdOx1 nCoV-19 vaccination against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/34276917/
- Thrombosis and severe acute respiratory syndrome Coronavirus 2 vaccines: vaccine-induced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34237213/.
- Renal vein thrombosis and pulmonary embolism secondary to vaccine-induced thrombotic immune thrombocytopenia (VITT): https://pubmed.ncbi.nlm.nih.gov/34268278/.
- Limb ischemia and pulmonary artery thrombosis after ChAdOx1 nCoV-19 vaccine (Oxford-AstraZeneca): a case of vaccine-induced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/33990339/.
- A case of vaccine-induced immune-immune thrombotic thrombocytopenia with massive arteriovenous thrombosis: https://pubmed.ncbi.nlm.nih.gov/34059191/
- Thrombocytopenia in an adolescent with sickle cell anemia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34331506/
- Vaccine-induced thrombocytopenia with severe headache: https://pubmed.ncbi.nlm.nih.gov/34525282/
- ChAdOx1 interacts with CAR and PF4 with implications for thrombosis with thrombocytopenia syndrome:https://www.science.org/doi/10.1126/sciadv.abl8213
- Lethal vaccine-induced immune thrombotic immune thrombocytopenia (VITT) following announcement 26.COV2.S: first documented case outside the U.S.: https://pubmed.ncbi.nlm.nih.gov/34626338/
- A prothrombotic thrombocytopenic disorder resembling heparin-induced thrombocytopenia after coronavirus-19 vaccination: https://europepmc.org/article/PPR/PPR304469 435.
- VITT (vaccine-induced immune thrombotic thrombocytopenia) after vaccination withChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34731555/
- Vaccine-induced immune thrombotic thrombocytopenia (VITT): a new clinicopathologic entity with heterogeneous clinical presentations: https://pubmed.ncbi.nlm.nih.gov/34159588/
- Treatment of acute ischemic stroke associated with ChAdOx1 nCoV-19 vaccineinduced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34461442/
- Cerebral venous sinus thrombosis after vaccination: the UK experience: https://pubmed.ncbi.nlm.nih.gov/34370974/
- Cerebral venous vein/venous sinus thrombosis with thrombocytopenia syndrome after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34373413/
- Portal vein thrombosis due to vaccine-induced immune thrombotic immune thrombocytopenia (VITT) after Covid vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34598301/
- Spontaneous HIT syndrome: knee replacement, infection and parallels with vaccineinduced immune thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34144250/
- Thrombocytopenia with acute ischemic stroke and hemorrhage in a patient recently vaccinated with an adenoviral vector-based COVID-19 vaccine:. https://pubmed.ncbi.nlm.nih.gov/33877737/
- ChAdOx1 nCoV-19 vaccine-associated thrombocytopenia: three cases of immune thrombocytopenia after 107,720 doses of ChAdOx1 vaccination in Thailand: https://pubmed.ncbi.nlm.nih.gov/34483267/.
- Pulmonary embolism, transient ischemic attack, and thrombocytopenia after Johnson & Johnson COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34261635/
- Neurosurgical considerations with respect to decompressive craniectomy for intracerebral hemorrhage after SARS-CoV-2 vaccination in vaccine-induced thrombotic thrombocytopenia-VITT: https://pubmed.ncbi.nlm.nih.gov/34202817/
- Secondary thrombocytopenia after SARS-CoV-2 vaccination: case report of haemorrhage and hematoma after minor oral surgery: https://pubmed.ncbi.nlm.nih.gov/34314875/.
- Venous thromboembolism and mild thrombocytopenia after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34384129/
- Fatal exacerbation of ChadOx1-nCoV-19-induced thrombotic thrombocytopenia syndrome after successful initial therapy with intravenous immunoglobulins: a rationale for monitoring immunoglobulin G levels: https://pubmed.ncbi.nlm.nih.gov/34382387/
- A rare case of COVID-19 vaccine-induced thrombotic thrombocytopenia (VITT) affecting the venosplanchnic and pulmonary arterial circulation from a UK district general hospital: https://pubmed.ncbi.nlm.nih.gov/34535492/
- COVID-19 vaccine-induced thrombotic thrombocytopenia: a case series: https://pubmed.ncbi.nlm.nih.gov/34527501/
- Immune thrombocytopenia after immunization with Vaxzevria ChadOx1-S vaccine (AstraZeneca), Victoria, Australia: https://pubmed.ncbi.nlm.nih.gov/34756770/
- Case report of immune thrombocytopenia after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34751013/.
- Thrombocytopenia with acute ischemic stroke and hemorrhage in a patient recently vaccinated with an adenoviral vector-based COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33877737/
- Intracerebral hemorrhage and thrombocytopenia after AstraZeneca COVID-19 vaccine: clinical and diagnostic challenges of vaccine-induced thrombotic thrombocytopenia: https://pubmed.ncbi.nlm.nih.gov/34646685/
- Thrombocytopenia, including immune thrombocytopenia after receiving COVID-19 mRNA vaccines reported to the Vaccine Adverse Event Reporting System (VAERS): https://pubmed.ncbi.nlm.nih.gov/34006408/
- Newly diagnosed immune thrombocytopenia in a pregnant patient after coronavirus disease 2019 vaccination: https://pubmed.ncbi.nlm.nih.gov/34420249/
- Thrombocytopenia in an adolescent with sickle cell anemia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34331506/
- Abdominal pain and bilateral adrenal hemorrhage from immune thrombotic thrombocytopenia induced by COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34546343/
- Venous thromboembolism and mild thrombocytopenia after ChAdOx1 nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34384129/.
100.Severe immune thrombocytopenia following COVID-19 vaccination: report of four cases and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34653943/.
101.Relapse of immune thrombocytopenia after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34591991/
102.Images of immune thrombotic thrombocytopenia induced by Oxford / AstraZeneca® COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33962903/.
103.Adenovirus interactions with platelets and coagulation and vaccine-induced immune thrombotic thrombocytopenia syndrome: https://pubmed.ncbi.nlm.nih.gov/34407607/
104.Complicated case report of long-term vaccine-induced thrombotic immune thrombocytopenia A: https://pubmed.ncbi.nlm.nih.gov/34835275/.
105.Prevalence of thrombocytopenia, anti-platelet factor 4 antibodies, and elevated Ddimer in Thais after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34568726/
106.Bilateral thalamic stroke: a case of COVID-19 (VITT) vaccine-induced immune thrombotic thrombocytopenia or a coincidence due to underlying risk factors: https://pubmed.ncbi.nlm.nih.gov/34820232/.
107.Successful treatment of vaccine-induced immune thrombotic thrombocytopenia in a 26-year-old female patient: https://pubmed.ncbi.nlm.nih.gov/34614491/
108.Case report: vaccine-induced immune thrombotic thrombocytopenia in a patient with pancreatic cancer after vaccination with messenger RNA-1273: https://pubmed.ncbi.nlm.nih.gov/34790684/
109.Vaccine-induced thrombotic thrombocytopenia after Ad26.COV2.S vaccination in a man presenting as acute venous thromboembolism: https://pubmed.ncbi.nlm.nih.gov/34096082/
110.Helms, J. M., Ansteatt, K. T., Roberts, J. C., Kamatam, S., Foong, K. S., Labayog, J. S., & Tarantino, M. D. (2021). Severe, Refractory Immune Thrombocytopenia Occurring After SARS-CoV-2 Vaccine. J Blood Med, 12, 221-224. doi:10.2147/JBM.S307047. https://www.ncbi.nlm.nih.gov/pubmed/33854395
111.Hippisley-Cox, J., Patone, M., Mei, X. W., Saatci, D., Dixon, S., Khunti, K., Coupland, C. A. C. (2021). Risk of thrombocytopenia and thromboembolism after covid-19 vaccination and SARS-CoV-2 positive testing: self-controlled case series study. BMJ, 374, n1931. doi:10.1136/bmj.n1931. https://www.ncbi.nlm.nih.gov/pubmed/34446426
112.Lee, E. J., Cines, D. B., Gernsheimer, T., Kessler, C., Michel, M., Tarantino, M. D., Bussel, J. B. (2021). Thrombocytopenia following Pfizer and Moderna SARSCoV-2 vaccination. Am J Hematol, 96(5), 534-537. doi:10.1002/ajh.26132. https://www.ncbi.nlm.nih.gov/pubmed/33606296
113.Welsh, K. J., Baumblatt, J., Chege, W., Goud, R., & Nair, N. (2021). Thrombocytopenia including immune thrombocytopenia after receipt of mRNA COVID-19 vaccines reported to the Vaccine Adverse Event Reporting System (VAERS). Vaccine, 39(25), 3329-3332. doi:10.1016/j.vaccine.2021.04.054. https://www.ncbi.nlm.nih.gov/pubmed/34006408
114.Relapse of immune thrombocytopenia after covid-19 vaccination in young male patient: https://pubmed.ncbi.nlm.nih.gov/34804803/.
115.Peduncular, symptomatic cavernous bleeding after immune thrombocytopenia induced SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34549178/.
ΑΙΜΟΡΡΑΓΙΚΕΣ ΔΙΑΤΑΡΑΧΕΣ
- Blood clots and bleeding episodes after BNT162b2 and ChAdOx1 nCoV-19 vaccination: analysis of European data: https://www.sciencedirect.com/science/article/pii/S0896841121000937
- Association between ChAdOx1 nCoV-19 vaccination and bleeding episodes: large population-based cohort study: https://pubmed.ncbi.nlm.nih.gov/34479760/.
Βαρείες Αιμορραγικές επιπλοκές (εγκεφαλικές, πνευμονικές, αμφιβληστροειδούς, των άκρων)
- Lobar hemorrhage with ventricular rupture shortly after the first dose of an mRNAbased SARS-CoV-2 vaccine: https://www.ncbi.nlm.nih.gov/labs/pmc/articles/PMC8553377/
- Retinal hemorrhage after SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34884407/.
- Lobar hemorrhage with ventricular rupture shortly after the first dose of a SARSCoV-2 mRNA-based SARS-CoV-2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34729467/
- Acral hemorrhage after administration of the second dose of SARS-CoV-2 vaccine. A post-vaccination reaction: https://pubmed.ncbi.nlm.nih.gov/34092400/742.
- Fatal cerebral hemorrhage after COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33928772/
- Intracerebral hemorrhage associated with vaccine-induced thrombotic thrombocytopenia after ChAdOx1 nCOVID-19 vaccination in a pregnant woman: https://pubmed.ncbi.nlm.nih.gov/34261297/
ΑΓΓΕΙΙΤΙΔΑ
- ANCA-associated vasculitis after Pfizer-BioNTech COVID-19 vaccine: https://www.sciencedirect.com/science/article/pii/S0272638621007423
- propylthiouracil-induced neutrophil anti-cytoplasmic antibody-associated vasculitis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34451967/
- IgA vasculitis in adult patient after vaccination with ChadOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34509658/
- A case of leukocytoclastic vasculitis after vaccination with a SARS-CoV2 vaccine:case report: https://pubmed.ncbi.nlm.nih.gov/34196469/
- A case of ANCA-associated vasculitis after AZD1222 (Oxford-AstraZeneca) SARSCoV-2 vaccination: victim or causality?: https://pubmed.ncbi.nlm.nih.gov/34416184/.
- A case of ANCA-associated vasculitis after AZD1222 (Oxford-AstraZeneca) SARSCoV-2 vaccination: victim or causality?: https://pubmed.ncbi.nlm.nih.gov/34416184/
- Leukocytoclastic vasculitis as a cutaneous manifestation of ChAdOx1 corona virus vaccine nCoV-19 (recombinant): https://pubmed.ncbi.nlm.nih.gov/34546608/
- Induction of cutaneous leukocytoclastic vasculitis after ChAdOx1 nCoV-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34853744/.
- Recurrent ANCA-associated vasculitis after Oxford AstraZeneca ChAdOx1-S COVID-19 vaccination: a case series of two patients: https://pubmed.ncbi.nlm.nih.gov/34755433/
- Cutaneous lymphocytic vasculitis after administration of the second dose of AZD1222 (Oxford-AstraZeneca) Severe acute respiratory syndrome Coronavirus 2 vaccine: chance or causality: https://pubmed.ncbi.nlm.nih.gov/34726187/.
- Case report: anti-neutrophil cytoplasmic antibody-associated vasculitis with acute renal failure and pulmonary hemorrhage can occur after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34859017/
- Intracerebral hemorrhage due to vasculitis following COVID-19 vaccination: case report: https://pubmed.ncbi.nlm.nih.gov/34783899/
- COVID-19 vaccine-induced urticarial vasculitis: https://pubmed.ncbi.nlm.nih.gov/34369046/.
- ANCA-associated vasculitis after Pfizer-BioNTech COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34280507/.
- New-onset leukocytoclastic vasculitis after COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34241833/
- Cutaneous small vessel vasculitis after COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34529877/.
- Outbreak of leukocytoclastic vasculitis after COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33928638/
- Leukocytoclastic vasculitis after exposure to COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34836739/
- Vasculitis and bursitis in [ 18 F] FDG-PET/CT after COVID-19 mRNA vaccine: post hoc ergo propter hoc?; https://pubmed.ncbi.nlm.nih.gov/34495381/.
- Cutaneous lymphocytic vasculitis after administration of COVID-19 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34327795
- Cutaneous leukocytoclastic vasculitis induced by Sinovac COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34660867/.
- Reactivation of IgA vasculitis after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34848431/
- Varicella-zoster virus-related small-vessel vasculitis after Pfizer-BioNTech COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34310759/.
- Imaging in vascular medicine: leukocytoclastic vasculitis after COVID-19 vaccine booster: https://pubmed.ncbi.nlm.nih.gov/34720009/
- Cutaneous vasculitis following COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34611627/.
- Possible case of COVID-19 mRNA vaccine-induced small-vessel vasculitis: https://pubmed.ncbi.nlm.nih.gov/34705320/.
- IgA vasculitis following COVID-19 vaccination in an adult: https://pubmed.ncbi.nlm.nih.gov/34779011/
- Propylthiouracil-induced anti-neutrophil cytoplasmic antibody-associated vasculitis following vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34451967/
- Coronavirus disease vaccine 2019 (COVID-19) in systemic lupus erythematosus and neutrophil anti-cytoplasmic antibody-associated vasculitis: https://pubmed.ncbi.nlm.nih.gov/33928459/
- Reactivation of IgA vasculitis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34250509/
- First description of immune complex vasculitis after COVID-19 vaccination with BNT162b2: case report: https://pubmed.ncbi.nlm.nih.gov/34530771/.
- Nephrotic syndrome and vasculitis after SARS-CoV-2 vaccine: true association or circumstantial: https://pubmed.ncbi.nlm.nih.gov/34245294/.
- Occurrence of de novo cutaneous vasculitis after vaccination against coronavirus disease (COVID-19): https://pubmed.ncbi.nlm.nih.gov/34599716/.
- Asymmetric cutaneous vasculitis after COVID-19 vaccination with unusual preponderance of eosinophils: https://pubmed.ncbi.nlm.nih.gov/34115904/.
- Granulomatous vasculitis after AstraZeneca anti-SARS-CoV-2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34237323/.
- A case of generalized Sweet’s syndrome with vasculitis triggered by recent vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34849386/
- Small-vessel vasculitis following Oxford-AstraZeneca vaccination against SARSCoV-2: https://pubmed.ncbi.nlm.nih.gov/34310763/
- Cutaneous vasculitis after severe acute respiratory syndrome coronavirus 2 vaccine: https://pubmed.ncbi.nlm.nih.gov/34557622/.
- Leukocytoclastic vasculitis after coronavirus disease vaccination 2019: https://pubmed.ncbi.nlm.nih.gov/34713472/803
- Outbreaks of mixed cryoglobulinemia vasculitis after vaccination against SARSCoV-2: https://pubmed.ncbi.nlm.nih.gov/34819272/
- Cutaneous small-vessel vasculitis after vaccination with a single dose of Janssen Ad26.COV2.S: https://pubmed.ncbi.nlm.nih.gov/34337124/
- Case of immunoglobulin A vasculitis after vaccination against coronavirus disease 2019: https://pubmed.ncbi.nlm.nih.gov/34535924/
- Relapse of microscopic polyangiitis after COVID-19 vaccination: case report: https://pubmed.ncbi.nlm.nih.gov/34251683/.
ΛΕΜΦΑΔΕΝΟΠΑΘΕΙΑ
- Rare case of contralateral supraclavicular lymphadenopathy after vaccination with COVID-19: computed tomography and ultrasound findings: https://pubmed.ncbi.nlm.nih.gov/34667486/
- COVID-19 mRNA vaccination-induced lymphadenopathy mimics lymphoma progression on FDG PET / CT: https://pubmed.ncbi.nlm.nih.gov/33591026/
- Lymphadenopathy in COVID-19 vaccine recipients: diagnostic dilemma in oncology patients: https://pubmed.ncbi.nlm.nih.gov/33625300/
- Hypermetabolic lymphadenopathy after administration of BNT162b2 mRNA vaccine Covid-19: incidence assessed by [ 18 F] FDG PET-CT and relevance for studyinterpretation: https://pubmed.ncbi.nlm.nih.gov/33774684/
- Lymphadenopathy after COVID-19 vaccination: review of imaging findings: https://pubmed.ncbi.nlm.nih.gov/33985872/
- Lymphadenopathy associated with COVID-19 vaccination on FDG PET/CT: distinguishing features in adenovirus-vectored vaccine: https://pubmed.ncbi.nlm.nih.gov/34115709/.
- COVID-19 vaccination-induced lymphadenopathy in a specialized breast imaging clinic in Israel: analysis of 163 cases: https://pubmed.ncbi.nlm.nih.gov/34257025/.
- Coronavirus disease vaccine 2019 mimics lymph node metastases in patients undergoing skin cancer follow-up: a single-center study: https://pubmed.ncbi.nlm.nih.gov/34280870/
- COVID-19 post-vaccination lymphadenopathy: report of fine-needle aspiration biopsy cytologic findings: https://pubmed.ncbi.nlm.nih.gov/34432391/
- Regional lymphadenopathy after COVID-19 vaccination: review of the literature and considerations for patient management in breast cancer care: https://pubmed.ncbi.nlm.nih.gov/34731748/
- Adverse events of COVID injection that may occur in children.Acute-onset supraclavicular lymphadenopathy coincident with intramuscular mRNA vaccination against COVID-19 may be related to the injection technique of the vaccine, Spain, January and February 2021: https://pubmed.ncbi.nlm.nih.gov/33706861/
- Supraclavicular lymphadenopathy after COVID-19 vaccination in Korea: serial followup by ultrasonography: https://pubmed.ncbi.nlm.nih.gov/34116295/
- Oxford-AstraZeneca COVID-19 vaccination induced lymphadenopathy on [18F] choline PET / CT, not just an FDG finding: https://pubmed.ncbi.nlm.nih.gov/33661328/
- A case of cervical lymphadenopathy following COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34141500/
- Unilateral lymphadenopathy after COVID-19 vaccination: a practical management plan for radiologists of all specialties: https://pubmed.ncbi.nlm.nih.gov/33713605/
- Supraclavicular lymphadenopathy after COVID-19 vaccination: an increasing presentation in the two-week wait neck lump clinic: https://pubmed.ncbi.nlm.nih.gov/33685772/
- COVID-19 vaccination and lower cervical lymphadenopathy in two-week neck lump clinic: a follow-up audit: https://pubmed.ncbi.nlm.nih.gov/33947605/.
- Cervical lymphadenopathy after coronavirus disease vaccination 2019: clinical features and implications for head and neck cancer services: https://pubmed.ncbi.nlm.nih.gov/34526175/
- Lymphadenopathy associated with the COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33786231/
- Evolution of lymphadenopathy on PET/MRI
- Massive cervical lymphadenopathy following vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34601889/
- Acute-onset supraclavicular lymphadenopathy coincident with intramuscular mRNA vaccination against COVID-19 may be related to the injection technique of the vaccine, Spain, January and February 2021: https://pubmed.ncbi.nlm.nih.gov/33706861/
- Supraclavicular lymphadenopathy after COVID-19 vaccination in Korea: serial followup by ultrasonography: https://pubmed.ncbi.nlm.nih.gov/34116295/
- A case of cervical lymphadenopathy following COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34141500/
- Unilateral lymphadenopathy after COVID-19 vaccination: a practical management plan for radiologists of all specialties: https://pubmed.ncbi.nlm.nih.gov/33713605/
- Supraclavicular lymphadenopathy after COVID-19 vaccination: an increasing presentation in the two-week wait neck lump clinic: https://pubmed.ncbi.nlm.nih.gov/33685772/
- COVID-19 vaccination and lower cervical lymphadenopathy in two-week neck lump clinic: a follow-up audit: https://pubmed.ncbi.nlm.nih.gov/33947605/.
- Cervical lymphadenopathy after coronavirus disease vaccination 2019: clinical features and implications for head and neck cancer services: https://pubmed.ncbi.nlm.nih.gov/34526175/
- Lymphadenopathy associated with the COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33786231/
- Evolution of lymphadenopathy on PET/MRI after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33625301/.
- Massive cervical lymphadenopathy following vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34601889/
- COVID-19 vaccine-related axillary and cervical lymphadenopathy in patients with current or previous breast cancer and other malignancies: cross-sectional imaging findings on MRI, CT and PET-CT: https://pubmed.ncbi.nlm.nih.gov/34719892/
- Evolution of Lymphadenopathy at Pet/MRI after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33625301/
Μασχαλιαία λεμφαδενοπάθεια
- COVID-19 vaccine-induced axillary and pectoral lymphadenopathy in PET: https://www.sciencedirect.com/science/article/pii/S1930043321002612
- Evolution of bilateral hypermetabolic axillary hypermetabolic lymphadenopathy on FDG PET/CT after 2-dose COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34735411/
- COVID-19 vaccine-related axillary lymphadenopathy in breast cancer patients: case series with literature review: https://pubmed.ncbi.nlm.nih.gov/34836672/.
- Subclinical axillary lymphadenopathy associated with COVID-19 vaccination on screening mammography: https://pubmed.ncbi.nlm.nih.gov/34906409/
- Axillary adenopathy associated with COVID-19 vaccination: imaging findings and follow-up recommendations in 23 women: https://pubmed.ncbi.nlm.nih.gov/33624520/
- Unilateral axillary adenopathy in the setting of COVID-19 vaccination: follow-up: https://pubmed.ncbi.nlm.nih.gov/34298342/
- COVID-19 vaccine-related axillary and cervical lymphadenopathy in patients with current or previous breast cancer and other malignancies: cross-sectional imaging findings on MRI, CT and PET-CT: https://pubmed.ncbi.nlm.nih.gov/34719892/
- Incidence of axillary adenopathy on breast imaging after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34292295/.
- Unilateral axillary lymphadenopathy related to COVID-19 vaccine: pattern on screening breast MRI allowing benign evaluation: https://pubmed.ncbi.nlm.nih.gov/34325221/
- Axillary lymphadenopathy in patients with recent Covid-19 vaccination: a new diagnostic dilemma: https://pubmed.ncbi.nlm.nih.gov/34825530/.
- COVID-19 vaccine-induced unilateral axillary adenopathy: follow-up evaluation in the USA: https://pubmed.ncbi.nlm.nih.gov/34655312/.
- Axillary adenopathy associated with COVID-19 vaccination: imaging findings and follow-up recommendations in 23 women: https://pubmed.ncbi.nlm.nih.gov/33624520/
- Unilateral axillary adenopathy in the setting of COVID-19 vaccination: follow-up: https://pubmed.ncbi.nlm.nih.gov/34298342/
- Incidence of axillary adenopathy on breast imaging after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34292295/.
- Unilateral axillary lymphadenopathy related to COVID-19 vaccine: pattern on screening breast MRI allowing benign evaluation: https://pubmed.ncbi.nlm.nih.gov/34325221/
- Axillary lymphadenopathy in patients with recent Covid-19 vaccination: a new diagnostic dilemma: https://pubmed.ncbi.nlm.nih.gov/34825530/.
- COVID-19 vaccine-induced unilateral axillary adenopathy: follow-up evaluation in the USA: https://pubmed.ncbi.nlm.nih.gov/34655312/.
- Adenopathy after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33625299/.
ΑΝΑΦΥΛΑΞΙΑ
- COVID-19 vaccine-associated anaphylaxis: a statement from the Anaphylaxis Committee of the World Allergy Organization:. https://www.sciencedirect.com/science/article/pii/S1939455121000119.
- Allergic reactions, including anaphylaxis, after receiving the first dose of the Pfizer-BioNTech COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33475702/
- Allergic reactions, including anaphylaxis, after receiving the first dose of Pfizer-BioNTech COVID-19 vaccine – United States, December 14-23, 2020: https://pubmed.ncbi.nlm.nih.gov/33444297/
- Allergic reactions, including anaphylaxis, after receiving first dose of Moderna COVID-19 vaccine – United States, December 21, 2020-January 10, 2021: https://pubmed.ncbi.nlm.nih.gov/33507892/
- Reports of anaphylaxis after coronavirus disease vaccination 2019, South Korea, February 26-April 30, 2021: https://pubmed.ncbi.nlm.nih.gov/34414880/
- Reports of anaphylaxis after receiving COVID-19 mRNA vaccines in the U.S.-Dec 14, 2020-Jan 18, 2021: https://pubmed.ncbi.nlm.nih.gov/33576785/
- Immunization practices and risk of anaphylaxis: a current, comprehensive update of COVID-19 vaccination data: https://pubmed.ncbi.nlm.nih.gov/34269740/
- Relationship between pre-existing allergies and anaphylactic reactions following administration of COVID-19 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34215453/
- Anaphylaxis Associated with COVID-19 mRNA Vaccines: Approach to Allergy Research: https://pubmed.ncbi.nlm.nih.gov/33932618/
- Allergic reactions and anaphylaxis to LNP-based COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/33571463/
- Cumulative adverse event report of anaphylaxis following injections of COVID-19 mRNA vaccine (Pfizer-BioNTech) in Japan: the first month report: https://pubmed.ncbi.nlm.nih.gov/34347278/
- COVID-19 vaccines increase the risk of anaphylaxis: https://pubmed.ncbi.nlm.nih.gov/33685103/
- Biphasic anaphylaxis after exposure to the first dose of the Pfizer-BioNTech COVID-19 mRNA vaccine COVID-19: https://pubmed.ncbi.nlm.nih.gov/34050949/
- Polyethylene glycol (PEG) is a cause of anaphylaxis to Pfizer / BioNTech mRNA COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33825239/
- Elevated rates of anaphylaxis after vaccination with Pfizer BNT162b2 mRNA vaccine against COVID-19 in Japanese healthcare workers; a secondary analysis of initial post-approval safety data: https://pubmed.ncbi.nlm.nih.gov/34128049/
- .IgE-mediated allergy to polyethylene glycol (PEG) as a cause of anaphylaxis to COVID-19 mRNA vaccines: https://pubmed.ncbi.nlm.nih.gov/34318537/
- Anaphylactic reactions to COVID-19 mRNA vaccines: a call for further studies: https://pubmed.ncbi.nlm.nih.gov/33846043/ 188.
- Anaphylaxis following Covid-19 vaccine in a patient with cholinergic urticaria: https://pubmed.ncbi.nlm.nih.gov/33851711/
- Anaphylaxis induced by CoronaVac COVID-19 vaccine: clinical features and results of revaccination: https://pubmed.ncbi.nlm.nih.gov/34675550/.
- Anaphylaxis after Moderna COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34734159/
- Sex differences in the incidence of anaphylaxis to LNP-mRNA vaccines COVID-19: https://pubmed.ncbi.nlm.nih.gov/34020815/
- Allergic reactions, including anaphylaxis, after receiving the first dose of Pfizer-BioNTech COVID-19 vaccine – United States, December 14 to 23, 2020: https://pubmed.ncbi.nlm.nih.gov/33641264/
- Allergic reactions, including anaphylaxis, after receiving the first dose of Moderna COVID-19 vaccine – United States, December 21, 2020 to January 10, 2021: https://pubmed.ncbi.nlm.nih.gov/33641268/
- Prolonged anaphylaxis to Pfizer 2019 coronavirus disease vaccine: a case report and mechanism of action: https://pubmed.ncbi.nlm.nih.gov/33834172/
- Anaphylaxis reactions to Pfizer BNT162b2 vaccine: report of 3 cases of anaphylaxis following vaccination with Pfizer BNT162b2: https://pubmed.ncbi.nlm.nih.gov/34579211/
- Biphasic anaphylaxis after first dose of 2019 messenger RNA coronavirus disease
vaccine with positive polysorbate 80 skin test result: https://pubmed.ncbi.nlm.nih.gov/34343674/
- Biphasic anaphylaxis after exposure to the first dose of Pfizer-BioNTech COVID-19 mRNA vaccine COVID-19: https://pubmed.ncbi.nlm.nih.gov/34050949/
- Biphasic anaphylaxis after exposure to the first dose of Pfizer-BioNTech COVID-19 mRNA vaccine COVID-19: https://pubmed.ncbi.nlm.nih.gov/34050949/
- Iguchi, T., Umeda, H., Kojima, M., Kanno, Y., Tanaka, Y., Kinoshita, N., & Sato, D. 2021). Cumulative Adverse Event Reporting of Anaphylaxis After mRNA COVID-19 Vaccine (Pfizer-BioNTech) Injections in Japan: The First-Month Report. Drug Saf, 44(11), 1209-1214. doi:10.1007/s40264-021-01104-9. https://www.ncbi.nlm.nih.gov/pubmed/34347278
- Team, C. C.-R., Food, & Drug, A. (2021). Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine – United States, December 14-23, 2020. MMWR Morb Mortal Wkly Rep, 70(2), 46-51. doi: 10.15585/mmwr.mm7002e1. https://www.ncbi.nlm.nih.gov/pubmed/33444297
ΑΛΛΕΡΓΙΕΣ
- An academic hospital experience assessing the risk of COVID-19 mRNA vaccine using patient’s allergy history: https://www.sciencedirect.com/science/article/pii/S2213219821007972
- Allergic reactions, including anaphylaxis, after receiving the first dose of the Pfizer-BioNTech COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33475702/
- Allergic reactions to the first COVID-19 vaccine: a potential role of polyethylene glycol: https://pubmed.ncbi.nlm.nih.gov/33320974/
- Pfizer Vaccine Raises Allergy Concerns: https://pubmed.ncbi.nlm.nih.gov/33384356/
- Allergic reactions, including anaphylaxis, after receiving the first dose of Pfizer-BioNTech COVID-19 vaccine – United States, December 14-23, 2020: https://pubmed.ncbi.nlm.nih.gov/33444297/
- Allergic reactions, including anaphylaxis, after receiving first dose of Moderna COVID-19 vaccine – United States, December 21, 2020-January 10, 2021: https://pubmed.ncbi.nlm.nih.gov/33507892/
- Severe Allergic Reactions after COVID-19 Vaccination with the Pfizer / BioNTech Vaccine in Great Britain and the USA: Position Statement of the German Allergy Societies: German Medical Association of Allergologists (AeDA), German Society for Allergology and Clinical Immunology (DGAKI) and Society for Pediatric Allergology and Environmental Medicine (GPA): https://pubmed.ncbi.nlm.nih.gov/33643776/
- Allergic reactions and anaphylaxis to LNP-based COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/33571463/
- Allergenic components of the mRNA-1273 vaccine for COVID-19: possible involvement of polyethylene glycol and IgG-mediated complement activation: https://pubmed.ncbi.nlm.nih.gov/33657648/
- Acute allergic reactions to COVID-19 mRNA vaccines: https://pubmed.ncbi.nlm.nih.gov/33683290/
- Polyethylene glycole allergy of the SARS CoV2 vaccine recipient: case report of a young adult recipient and management of future exposure to SARS-CoV2: https://pubmed.ncbi.nlm.nih.gov/33919151/
- Allergic reactions and adverse events associated with administration of mRNA-based vaccines. A health system experience: https://pubmed.ncbi.nlm.nih.gov/34474708/
- Allergic reactions to COVID-19 vaccines: statement of the Belgian Society of Allergy and Clinical Immunology (BelSACI): https://www.tandfonline.com/doi/abs/10.1080/17843286.2021.1909447
- Allergic reactions after COVID-19 vaccination: putting the risk in perspective: https://pubmed.ncbi.nlm.nih.gov/34463751/
- Risk of severe allergic reactions to COVID-19 vaccines among patients with allergic skin disease: practical recommendations. An ETFAD position statement with external experts: https://pubmed.ncbi.nlm.nih.gov/33752263/
- Association of self-reported history of high-risk allergy with allergy symptoms after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34698847/
- Greenhawt, M., Abrams, E. M., Shaker, M., Chu, D. K., Khan, D., Akin, C., Golden, D. B. K. (2021). The Risk of Allergic Reaction to SARS-CoV-2 Vaccines and Recommended Evaluation and Management: A Systematic Review, Meta-Analysis, GRADE Assessment, and International Consensus Approach. J Allergy Clin Immunol
Pract, 9(10), 3546-3567. doi:10.1016/j.jaip.2021.06.006. https://www.ncbi.nlm.nih.gov/pubmed/34153517
- Klimek, L., Bergmann, K. C., Brehler, R., Pfutzner, W., Zuberbier, T., Hartmann, K., Worm, M. (2021). Practical handling of allergic reactions to COVID-19 vaccines: A position paper from German and Austrian Allergy Societies AeDA, DGAKI, GPA and OGAI. Allergo J Int, 1-17. doi:10.1007/s40629-021-00165-7. https://www.ncbi.nlm.nih.gov/pubmed/33898162
- Klimek, L., Novak, N., Hamelmann, E., Werfel, T., Wagenmann, M., Taube, C., Worm, M. (2021). Severe allergic reactions after COVID-19 vaccination with the Pfizer/BioNTech vaccine in Great Britain and USA: Position statement of the German Allergy Societies: Medical Association of German Allergologists (AeDA), German Society for Allergology and Clinical Immunology (DGAKI) and Society for Pediatric Allergology and Environmental Medicine (GPA). Allergo J Int, 30(2), 51-55. doi: 10.1007/s40629-020-00160-4. https://www.ncbi.nlm.nih.gov/pubmed/33643776
- Warren, C. M., Snow, T. T., Lee, A. S., Shah, M. M., Heider, A., Blomkalns, A., Nadeau, K. C. (2021). Assessment of Allergic and Anaphylactic Reactions to mRNA COVID-19 Vaccines With Confirmatory Testing in a US Regional Health System. JAMA Netw Open, 4(9), e2125524. doi:10.1001/jamanetworkopen.2021.25524. https://www.ncbi.nlm.nih.gov/pubmed/34533570
- Kounis NG, Koniari I, de Gregorio C, Velissaris D, Petalas K, Brinia A, et al. Allergic Reactions to Current Available COVID-19 Vaccinations: Pathophysiology, Causality, and Therapeutic Considerations. Vaccines (Basel). 2021;9(3).
ΝΕΥΡΟΛΟΓΙΚΕΣ ΔΙΑΤΑΡΑΧΕΣ
- Neurological symptoms and neuroimaging alterations related to COVID-19 vaccine: cause or coincidence?: https://pubmed.ncbi.nlm.nih.gov/34507266/
- Spectrum of neurological complications after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34719776/.
- Ιn-hospital observational study of neurological disorders in patients recently vaccinated with COVID-19 mRNA vaccines: https://pubmed.ncbi.nlm.nih.gov/34688190/
- Neurological side effects of SARS-CoV-2 vaccines: https://pubmed.ncbi.nlm.nih.gov/34750810/
- Neurological complications after the first dose of COVID-19 vaccines and SARSCoV-2 infection: https://pubmed.ncbi.nlm.nih.gov/34697502/
- Nerve and muscle adverse events after vaccination with COVID-19: a systematic review and meta-analysis of clinical trials: https://pubmed.ncbi.nlm.nih.gov/34452064/.
Ενδοκρανιακή αιμορραγία, αγγειακό εγκεφαλικό επεισόδιο
- Intracerebral haemorrhage due to thrombosis with thrombocytopenia syndrome after COVID-19 vaccination: the first fatal case in Korea: https://pubmed.ncbi.nlm.nih.gov/34402235/
- Intracerebral haemorrhage twelve days after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34477089/
- Neurosurgical considerations regarding decompressive craniectomy for intracerebral hemorrhage after SARS-CoV-2 vaccination in vaccine-induced thrombotic thrombocytopenia-VITT: https://pubmed.ncbi.nlm.nih.gov/34202817/
- First dose of ChAdOx1 and BNT162b2 COVID-19 vaccines and thrombocytopenic, thromboembolic, and hemorrhagic events in Scotland: https://pubmed.ncbi.nlm.nih.gov/34108714/
- Large hemorrhagic stroke after vaccination against ChAdOx1 nCoV-19: a case report: https://pubmed.ncbi.nlm.nih.gov/34273119/
- Major hemorrhagic stroke after ChAdOx1 nCoV-19 vaccination: a case report: https://pubmed.ncbi.nlm.nih.gov/34273119/
- Aphasia seven days after the second dose of an mRNA-based SARS-CoV-2 vaccine. Brain MRI revealed an intracerebral haemorrhage (ICBH) in the left temporal lobe in a 52-year-old man. https://www.sciencedirect.com/science/article/pii/S2589238X21000292#f0005
- Incidence of acute ischemic stroke after coronavirus vaccination in Indonesia: case series: https://pubmed.ncbi.nlm.nih.gov/34579636/
- Fatal brain haemorrhage after COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33928772/
Σύνδρομο Guillain-Barré
- GM1 ganglioside antibody and COVID-19-related Guillain Barre syndrome: case report, systemic review, and implications for vaccine development: https://www.sciencedirect.com/science/article/pii/S2666354621000065
- Guillain-Barré syndrome after AstraZeneca COVID-19 vaccination: causal or casual association: https://www.sciencedirect.com/science/article/pii/S0303846721004169
- Sensory Guillain-Barré syndrome after ChAdOx1 nCov-19 vaccine: report of two cases and review of the literature: https://www.sciencedirect.com/science/article/pii/S0165572821002186
- Guillain-Barré syndrome after the first dose of SARS-CoV-2 vaccine: a temporary occurrence, not a causal association: https://www.sciencedirect.com/science/article/pii/S2214250921000998.
- Guillain-Barré syndrome presenting as facial diplegia after vaccination with COVID-19: a case report: https://www.sciencedirect.com/science/article/pii/S0736467921006442
- Guillain-Barré syndrome after the first injection of ChAdOx1 nCoV-19 vaccine: first report: https://www.sciencedirect.com/science/article/pii/S0035378721005853.
- SARS-CoV-2 vaccines are not safe for those with Guillain-Barre syndrome following vaccination: https://www.sciencedirect.com/science/article/pii/S2049080121005343
- Guillian Barré syndrome after vaccination with mRNA-1273 against COVID-19: https://pubmed.ncbi.nlm.nih.gov/34477091/
- A novel case of bifacial diplegia variant of Guillain-Barré syndrome after vaccination with Janssen COVID-19: https://pubmed.ncbi.nlm.nih.gov/34449715/
- Sensory Guillain-Barré syndrome following ChAdOx1 nCov-19 vaccine: report of two cases and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34416410/.
- Facial diplegia: a rare and atypical variant of Guillain-Barré syndrome and the Ad26.COV2.S vaccine: https://pubmed.ncbi.nlm.nih.gov/34447646/
- Guillain-Barré syndrome after ChAdOx1 nCoV-19 COVID-19 vaccination: a case series: https://pubmed.ncbi.nlm.nih.gov/34548920/
- AstraZeneca COVID-19 vaccine and Guillain-Barré syndrome in Tasmania: a causal link: https://pubmed.ncbi.nlm.nih.gov/34560365/
- COVID-19, Guillain-Barré and vaccineA dangerous mix: https://pubmed.ncbi.nlm.nih.gov/34108736/.
- Guillain-Barré syndrome after the first dose of Pfizer-BioNTech COVID-19 vaccine: case report and review of reported cases: https://pubmed.ncbi.nlm.nih.gov/34796417/.
- Guillain-Barre syndrome after BNT162b2 COVID-19 vaccine: https://link.springer.com/article/10.1007%2Fs10072-021-05523-5.
- COVID-19 adenovirus vaccines and Guillain-Barré syndrome with facial palsy: https://onlinelibrary.wiley.com/doi/10.1002/ana.26258.
- Association of receipt association of Ad26.COV2.S COVID-19 vaccine with presumed Guillain-Barre syndrome, February-July 2021: https://jamanetwork.com/journals/jama/fullarticle/2785009
- A case of Guillain-Barré syndrome after Pfizer COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34567447/
- Guillain-Barré syndrome associated with COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34648420/.
- Rate of recurrent Guillain-Barré syndrome after COVID-19 BNT162b2 mRNA vaccine: https://jamanetwork.com/journals/jamaneurology/fullarticle/2783708
- Guillain-Barre syndrome after COVID-19 vaccination in an adolescent: https://www.pedneur.com/article/S0887-8994(21)00221-6/fulltext.
- Guillain-Barre syndrome after ChAdOx1-S / nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34114256/.
- Guillain-Barre syndrome after COVID-19 mRNA-1273 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34767184/.
- Guillain-Barre syndrome following SARS-CoV-2 vaccination in 19 patients: https://pubmed.ncbi.nlm.nih.gov/34644738/.
- Guillain-Barre syndrome presenting with facial diplegia following vaccination with COVID-19 in two patients: https://pubmed.ncbi.nlm.nih.gov/34649856/
- A rare case of Guillain-Barré syndrome after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34671572/
- Neurological complications of COVID-19: Guillain-Barre syndrome after Pfizer COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/33758714/
- COVID-19 vaccine causing Guillain-Barre syndrome, an uncommon potential side effect: https://pubmed.ncbi.nlm.nih.gov/34484780/
- Guillain-Barre syndrome after the first dose of COVID-19 vaccination: case report; https://pubmed.ncbi.nlm.nih.gov/34779385/.
- Guillain-Barre syndrome after the first injection of ChAdOx1 nCoV-19 vaccine: first report: https://pubmed.ncbi.nlm.nih.gov/34217513/.
- A case of sensory ataxic Guillain-Barre syndrome with immunoglobulin G anti-GM1 antibodies after first dose of COVID-19 BNT162b2 mRNA vaccine (Pfizer): https://pubmed.ncbi.nlm.nih.gov/34871447/
- A variant of Guillain-Barré syndrome after SARS-CoV-2 vaccination: AMSAN: https://pubmed.ncbi.nlm.nih.gov/34370408/.
- A rare variant of Guillain-Barré syndrome after vaccination with Ad26.COV2.S: https://pubmed.ncbi.nlm.nih.gov/34703690/.
- Guillain-Barré syndrome after SARS-CoV-2 vaccination in a patient with previous vaccine-associated Guillain-Barré syndrome: https://pubmed.ncbi.nlm.nih.gov/34810163/
- Guillain-Barré syndrome in an Australian state using mRNA and adenovirus-vector SARS-CoV-2 vaccines: https://onlinelibrary.wiley.com/doi/10.1002/ana.26218
- Variant Guillain-Barré syndrome occurring after SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34114269/
- Guillian-Barre syndrome with axonal variant temporally associated with Moderna SARS-CoV-2 mRNA-based vaccine: https://pubmed.ncbi.nlm.nih.gov/34722067/
- Guillain-Barre syndrome after the first dose of SARS-CoV-2 vaccine: a temporary occurrence, not a causal association: https://pubmed.ncbi.nlm.nih.gov/33968610/
- SARS-CoV-2 vaccines can be complicated not only by Guillain-Barré syndrome but also by distal small fiber neuropathy: https://pubmed.ncbi.nlm.nih.gov/34525410/
- Clinical variant of Guillain-Barré syndrome with prominent facial diplegia after AstraZeneca 2019 coronavirus disease vaccine: https://pubmed.ncbi.nlm.nih.gov/34808658/
- Miller-Fisher syndrome and Guillain-Barré syndrome overlap syndrome in a patient after Oxford-AstraZeneca SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34848426/
- Bilateral facial weakness with a variant of paresthesia of Guillain-Barre syndrome after Vaxzevria COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34261746/
Οξεία υπερενεργός εγκεφαλοπάθεια, εγκεφαλομυελίτιδα
- Acute hyperactive encephalopathy following COVID-19 vaccination with dramatic response to methylprednisolone: a case report: https://www.sciencedirect.com/science/article/pii/S2049080121007536
- Post-vaccinal encephalitis after ChAdOx1 nCov-19: https://pubmed.ncbi.nlm.nih.gov/34324214/
- Acute disseminated encephalomyelitis following vaccination against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/34325334/
- Acute hyperactive encephalopathy following COVID-19 vaccination with dramatic response to methylprednisolone: case report: https://pubmed.ncbi.nlm.nih.gov/34512961/
Παράλυση του Bell
- Bell’s palsy and SARS-CoV-2 vaccines: an unfolding story: https://www.sciencedirect.com/science/article/pii/S1473309921002735
- Bell’s palsy after the second dose of the Pfizer COVID-19 vaccine in a patient with a history of recurrent Bell’s palsy: https://www.sciencedirect.com/science/article/pii/S266635462100020X
- Bell’s palsy after COVID-19 vaccination: case report: https://www.sciencedirect.com/science/article/pii/S217358082100122X.
- The association between COVID-19 vaccination and Bell’s palsy: https://pubmed.ncbi.nlm.nih.gov/34411533/
- Bell’s palsy after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/33611630/
- Bell’s palsy after 24 hours of mRNA-1273 SARS-CoV-2 mRNA-1273 vaccine: https://pubmed.ncbi.nlm.nih.gov/34336436/
- Bell’s palsy after Ad26.COV2.S COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34014316/
- Bell’s palsy after COVID-19 vaccination: case report: https://pubmed.ncbi.nlm.nih.gov/34330676/
- Acute facial paralysis as a possible complication of SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/33975372/.
- Bell’s palsy after COVID-19 vaccination with high antibody response in CSF: https://pubmed.ncbi.nlm.nih.gov/34322761/.
- Bell’s palsy after a single dose of vaccine mRNA. SARS-CoV-2: case report: https://pubmed.ncbi.nlm.nih.gov/34032902/.
- Adverse event reporting and risk of Bell’s palsy after COVID-19 vaccination: https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(21)00646-0/fulltext.
- Bilateral facial nerve palsy and COVID-19 vaccination: causality or coincidence:https://pubmed.ncbi.nlm.nih.gov/34522557/
- Left Bell’s palsy after the first dose of mRNA-1273 SARS-CoV-2 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34763263/.
- Bell’s palsy after inactivated vaccination with COVID-19 in a patient with a history of recurrent Bell’s palsy: case report: https://pubmed.ncbi.nlm.nih.gov/34621891/
- Bell’s palsy after vaccination with mRNA (BNT162b2) and inactivated (CoronaVac) SARS-CoV-2 vaccines: a case series and a nested case-control study: https://pubmed.ncbi.nlm.nih.gov/34411532/
- A case of acute demyelinating polyradiculoneuropathy with bilateral facial palsy after ChAdOx1 nCoV-19 vaccine:. https://pubmed.ncbi.nlm.nih.gov/34272622/
- Type I interferons as a potential mechanism linking COVID-19 mRNA vaccines with Bell’s palsy: https://pubmed.ncbi.nlm.nih.gov/33858693/
- Facial nerve palsy following administration of COVID-19 mRNA vaccines: analysis of self-report database: https://www.sciencedirect.com/science/article/pii/S1201971221007049
- COVID-19 vaccination association and facial nerve palsy: A case-control study: https://pubmed.ncbi.nlm.nih.gov/34165512/
- Sequential contralateral facial nerve palsy after first and second doses of COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34281950/.
- Peripheral facial nerve palsy after vaccination with BNT162b2 (COVID-19): https://pubmed.ncbi.nlm.nih.gov/33734623/
- Facial nerve palsy after administration of COVID-19 mRNA vaccines: analysis of selfreport database: https://pubmed.ncbi.nlm.nih.gov/34492394/
- A case of acute demyelinating polyradiculoneuropathy with bilateral facial palsy following ChAdOx1 nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34272622
Οξεία μυελίτιδα και εγκάρσια μυελίτιδα
- Acute myelitis and ChAdOx1 nCoV-19 vaccine: coincidental or causal association: https://www.sciencedirect.com/science/article/pii/S0165572821002137
- Acute transverse myelitis (ATM): clinical review of 43 patients with COVID-19-associated ATM and 3 serious adverse events of post-vaccination ATM with ChAdOx1 nCoV-19 vaccine (AZD1222): https://pubmed.ncbi.nlm.nih.gov/33981305/
- Transverse myelitis induced by SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34458035/
- Acute transverse myelitis (ATM): clinical review of 43 patients with COVID-19-associated ATM and 3 serious adverse events of post-vaccination ATM with ChAdOx1 nCoV-19 (AZD1222) vaccine: https://pubmed.ncbi.nlm.nih.gov/33981305/.
- Acute transverse myelitis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34684047/.
- Extensive longitudinal transverse myelitis after ChAdOx1 nCOV-19 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34641797/.
- Acute transverse myelitis after SARS-CoV-2 vaccination: case report and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34482455/.
- Acute transverse myelitis following inactivated COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34370410/
- Acute transverse myelitis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34579245/.
- A case of longitudinally extensive transverse myelitis following Covid-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34182207/
- Post COVID-19 transverse myelitis; a case report with review of the literature: https://pubmed.ncbi.nlm.nih.gov/34457267/.
- Acute bilateral bilateral optic neuritis/chiasm with longitudinal extensive transverse myelitis in long-standing stable multiple sclerosis after vector-based vaccination against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/34131771/
- Extensive longitudinal transverse myelitis following AstraZeneca COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34507942/.
- Longitudinally extensive cervical myelitis after vaccination with inactivated virus based COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34849183/
Πολλαπλή σκλήρυνση
- Severe relapse of multiple sclerosis after COVID-19 vaccination: a case report: https://pubmed.ncbi.nlm.nih.gov/34447349/
- Acute relapse and impaired immunization after COVID-19 vaccination in a patient with multiple sclerosis treated with rituximab: https://pubmed.ncbi.nlm.nih.gov/34015240
- Humoral response induced by Prime-Boost vaccination with ChAdOx1 nCoV-19 and BNT162b2 mRNA vaccines in a patient with multiple sclerosis treated with teriflunomide: https://pubmed.ncbi.nlm.nih.gov/34696248/
Οξείες φλεγμονώδεις νευροπάθειες
- Reporting of acute inflammatory neuropathies with COVID-19 vaccines: subgroup disproportionality analysis in VigiBase: https://pubmed.ncbi.nlm.nih.gov/34579259/
Vogt-Koyanagi-Harada syndrome
- Vogt-Koyanagi-Harada syndrome after COVID-19 and ChAdOx1 nCoV-19 (AZD1222) vaccination: https://pubmed.ncbi.nlm.nih.gov/34462013/.
- Reactivation of Vogt-Koyanagi-Harada disease under control for more than 6 years, after anti-SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34224024/
Miller Fisher Syndrome
- Miller Fisher syndrome after Pfizer COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34817727/.
- Miller Fisher syndrome after 2019 BNT162b2 mRNA coronavirus vaccination: https://pubmed.ncbi.nlm.nih.gov/34789193/.
Ανθεκτικό Status Epilepticus
- New-onset refractory status epilepticus after chadox1 ncov-19 vaccination: https://www.sciencedirect.com/science/article/pii/s0165572821001569
Νόσος από Prion (σπογγώδης εγκεφαλοπάθεια)
- COVID-19 RNA-based vaccines and the risk of prion disease: https://scivisionpub.com/pdfs/covid19rna-based-vaccines-and-the-risk-of-prion-disease-1503.pdf
Φλεγμονή Κεντρικού Νευρικού Συστήματος
- COVID-19 mRNA vaccine causing CNS inflammation: a case series: https://link.springer.com/article/10.1007/s00415-021-10780-7
Απομυελίνωση Κεντρικού Νευρικού Συστήματος
- A systematic review of cases of CNS demyelination following COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34839149/
Οπτικοκινητική παράλυση
- Transient oculomotor paralysis after administration of RNA-1273 messenger vaccine for SARS-CoV-2 diplopia after COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/
34369471/
Σύνδρομο Parsonage-Turner
- Parsonage-Turner syndrome associated with SARS-CoV-2 or SARS-CoV-2 vaccination. Comment on: “Neuralgic amyotrophy and COVID-19 infection: 2 cases of accessory spinal nerve palsy” by Coll et al. Articular Spine 2021; 88: 10519: https://pubmed.ncbi.nlm.nih.gov/34139321/.
Tolosa-Hunt syndrome
- Tolosa-Hunt syndrome occurring after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34513398/
Μυατροφική νευραλγία
- Amyotrophic Neuralgia secondary to Vaxzevri vaccine (AstraZeneca) COVID-19: https://pubmed.ncbi.nlm.nih.gov/34330677/
Νευρολογική φαντοσμία
- Unique imaging findings of neurologic phantosmia after Pfizer-BioNtech COVID-19 vaccination: a case report: https://pubmed.ncbi.nlm.nih.gov/34096896/
Στοματοπροσωπική μυολειτουργική διαταραχή
- Reported orofacial adverse effects from COVID-19 vaccines: the known and the unknown: https://pubmed.ncbi.nlm.nih.gov/33527524/
Οξεία ημιχορεία–ημιβαλλισμός
- Acute hemichorea-hemibalismus after COVID-19 (AZD1222) vaccination: https://pubmed.ncbi.nlm.nih.gov/34581453/
Πονοκέφαλος
- Headache attributed to COVID-19 (SARS-CoV-2 coronavirus) vaccination with the ChAdOx1 nCoV-19 (AZD1222) vaccine: a multicenter observational cohort study: https://pubmed.ncbi.nlm.nih.gov/34313952/
Αισθητικονευρική απώλεια ακοής
- Sudden sensorineural hearing loss after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34670143/.
Ευρήματα νευροαπεικόνισης μετά από εμβολιασμό για COVID-19
- Spectrum of neuroimaging findings in post-CoVID-19 vaccination: a case series and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34842783/
Κατάθλιψη
- Depression after ChAdOx1-S / nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34608345/.
ΟΦΘΑΛΜΟΛΟΓΙΚΕΣ ΒΛΑΒΕΣ
- Ocular adverse events following COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34559576/
Οξεία νευροαμφιβληστροειδοπάθεια της ωχράς κηλίδας
- Bilateral acute macular neuroretinopathy after SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34287612/
Οπτική Νευρομυελίτιδα
- Beware of neuromyelitis optica spectrum disorder after vaccination with inactivated virus for COVID-19: https://pubmed.ncbi.nlm.nih.gov/34189662/
- Neuromyelitis optica in a healthy woman after vaccination against severe acute respiratory syndrome coronavirus 2 mRNA-1273: https://pubmed.ncbi.nlm.nih.gov/34660149/
Κεντρική Ορώδης Αμφιβληστροειδοπάθεια
- Acute-onset central serous retinopathy after immunization with COVID-19 mRNA vaccine:. https://www.sciencedirect.com/science/article/pii/S2451993621001456.
Απόφραξη κεντρικής φλέβας του αμφιβληστροειδούς
- Central retinal vein occlusion after vaccination with SARS-CoV-2 mRNA: case report:
https://pubmed.ncbi.nlm.nih.gov/34571653/.
Χοριοειδίτιδα
- Bilateral uveitis after inoculation with COVID-19 vaccine: a case report: https://www.sciencedirect.com/science/article/pii/S1201971221007797
Κερατόλυση
- Bilateral immune-mediated keratolysis after immunization with SARS-CoV-2 recombinant viral vector vaccine: https://pubmed.ncbi.nlm.nih.gov/34483273/.
ΠΟΛΥΣΥΣΤΗΜΑΤΙΚΟ ΦΛΕΓΜΟΝΩΔΕΣ ΣΥΝΔΡΟΜΟ
- Post-vaccination multisystem inflammatory syndrome in adults without evidence of prior SARS-CoV-2 infection: https://pubmed.ncbi.nlm.nih.gov/34852213/
- Buchhorn, R., Meyer, C., Schulze-Forster, K., Junker, J., & Heidecke, H. (2021). Autoantibody Release in Children after Corona Virus mRNA Vaccination: A Risk Factor of Multisystem Inflammatory Syndrome? Vaccines (Basel), 9(11). doi:10.3390/vaccines9111353. https://www.ncbi.nlm.nih.gov/pubmed/34835284
- Chai, Q., Nygaard, U., Schmidt, R. C., Zaremba, T., Moller, A. M., & Thorvig, C. M. (2022). Multisystem inflammatory syndrome in a male adolescent after his second Pfizer-BioNTech COVID-19 vaccine. Acta Paediatr, 111(1), 125-127. doi:10.1111/apa.16141.
ΣΥΝΔΡΟΜΟ ΔΙΑΦΥΓΗΣ ΤΡΙΧΟΕΙΔΩΝ
- Fatal systemic capillary leak syndrome after SARS-COV-2 vaccination in a patient with multiple myeloma: https://pubmed.ncbi.nlm.nih.gov/34459725/
- Systemic capillary leak syndrome after ChAdOx1 nCOV-19 (Oxford-AstraZeneca) vaccination https://pubmed.ncbi.nlm.nih.gov/34362727/
- Systemic capillary extravasation syndrome following vaccination with ChAdOx1 nCOV-19 (Oxford-AstraZeneca): https://pubmed.ncbi.nlm.nih.gov/34362727/
ΕΞΑΡΣΗ/ΕΜΦΑΝΙΣΗ ΑΥΤΟΑΝΟΣΩΝ ΝΟΣΗΜΑΤΩΝ
- Immune-mediated disease outbreaks or recent-onset disease in 27 subjects after mRNA/DNA vaccination against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/33946748/
- Severe autoimmune hemolytic autoimmune anemia after receiving SARS-CoV-2 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34549821/
- Severe autoimmune hemolytic anemia after receipt of SARS-CoV-2 mRNA vaccine:
https://onlinelibrary.wiley.com/doi/10.1111/trf.16672
- Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study https://www.ncbi.nlm.nih.gov/pubmed/34127481
- Autoimmune encephalitis after ChAdOx1-S SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34846583/
- Immune-mediated disease outbreaks or new-onset disease in 27 subjects after mRNA/DNA vaccination against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/33946748/
- Neurological autoimmune diseases after SARS-CoV-2 vaccination: a case series: https://pubmed.ncbi.nlm.nih.gov/34668274/.
Αυτοάνοσες φλεγμονώδεις ρευματοπάθειες
- Furer, V., Eviatar, T., Zisman, D., Peleg, H., Paran, D., Levartovsky, D., . . . Elkayam, O. (2021). Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis, 80(10), 1330-1338. doi:10.1136/
annrheumdis-2021-220647. https://www.ncbi.nlm.nih.gov/pubmed/34127481
Νόσος του Still
- An outbreak of Still’s disease after COVID-19 vaccination in a 34-year-old patient: https://pubmed.ncbi.nlm.nih.gov/34797392/
Συστηματικός Ερυθηματώδης Λύκος
- Induction and exacerbation of subacute cutaneous lupus erythematosus after mRNA- or adenoviral vector-based SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34291477/
- Ntouros, P. A., Vlachogiannis, N. I., Pappa, M., Nezos, A., Mavragani, C. P., Tektonidou, M. G., Sfikakis, P. P. (2021). Effective DNA damage response after acute but not chronic immune challenge: SARS-CoV-2 vaccine versus Systemic
Lupus Erythematosus. Clin Immunol, 229, 108765. doi:10.1016/j.clim.2021.108765.
https://www.ncbi.nlm.nih.gov/pubmed/34089859
Αυτοάνοση ηπατίτιδα
- Autoimmune hepatitis developing after coronavirus disease vaccine 2019 (COVID-19): causality or victim?: https://pubmed.ncbi.nlm.nih.gov/33862041/
- Autoimmune hepatitis triggered by vaccination against SARS-CoV-2: https://pubmed.ncbi.nlm.nih.gov/34332438/
- Acute autoimmune-like hepatitis with atypical antimitochondrial antibody after vaccination with COVID-19 mRNA: a new clinical entity: https://pubmed.ncbi.nlm.nih.gov/34293683/.
- Autoimmune hepatitis after COVID vaccine: https://pubmed.ncbi.nlm.nih.gov/34225251/
- Hepatitis C virus reactivation after COVID-19 vaccination: a case report: https://pubmed.ncbi.nlm.nih.gov/34512037/
- Autoimmune hepatitis developing after ChAdOx1 nCoV-19 vaccine (Oxford-AstraZeneca): https://pubmed.ncbi.nlm.nih.gov/34171435/
- Autoimmune hepatitis triggered by SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34332438/.
- Immune-mediated hepatitis with the Moderna vaccine is no longer a coincidence but confirmed: https://www.sciencedirect.com/science/article/pii/S0168827821020936
Πορφύρα Henoch-Schonlein
- A rare case of Henoch-Schönlein purpura after a case report of COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34518812/
- Henoch-Schönlein purpura occurring after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34247902/.
- Henoch-Schönlein purpura following the first dose of COVID-19 viral vector vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34696186/.
Αιμοφαγοκυτταρική λεμφοιστιοκυττάρωση
- Hemophagocytic lymphohistiocytosis after vaccination with ChAdOx1 nCov-19: https://pubmed.ncbi.nlm.nih.gov/34406660/.
- Hemophagocytic lymphohistiocytosis following COVID-19 vaccination (ChAdOx1 nCoV-19): https://pubmed.ncbi.nlm.nih.gov/34862234/
ΙΣΤΟΠΑΘΟΛΟΓΙΚΑ ΕΥΡΗΜΑΤΑ ΝΕΚΡΟΤΟΜΩΝ
- Sessa, F., Salerno, M., Esposito, M., Di Nunno, N., Zamboni, P., & Pomara, C. (2021). Autopsy Findings and Causality Relationship between Death and COVID-19 Vaccination: A Systematic Review. J Clin Med, 10(24). doi:10.3390/jcm10245876. https://www.ncbi.nlm.nih.gov/pubmed/34945172
- Post-mortem investigation of deaths after vaccination with COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34591186/
- A look at the role of postmortem immunohistochemistry in understanding the inflammatory pathophysiology of COVID-19 disease and vaccine-related thrombotic adverse events: a narrative review: https://pubmed.ncbi.nlm.nih.gov/34769454/
- COVID-19 vaccine and death: causality algorithm according to the WHO eligibility diagnosis: https://pubmed.ncbi.nlm.nih.gov/34073536/
- Post-mortem investigation of deaths after vaccination with COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34591186/
ΡΑΒΔΟΜΥΟΛΥΣΗ
- Rhabdomyolysis and fasciitis induced by the COVID-19 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34435250/
- COVID-19 vaccine-induced rhabdomyolysis: case report with literature review: https://pubmed.ncbi.nlm.nih.gov/34186348/
- COVID-19 vaccine-induced rhabdomyolysis: case report with review of the literature:
https://www.sciencedirect.com/science/article/pii/S1871402121001880
- Rhabdomyolysis and fasciitis induced by COVID-19 mRNA vaccine: https://pubmed.ncbi.nlm.nih.gov/34435250/.
- Case report: ANCA-associated vasculitis presenting with rhabdomyolysis and crescentic Pauci-Inmune glomerulonephritis after vaccination with Pfizer-BioNTech COVID-19 mRNA: https://pubmed.ncbi.nlm.nih.gov/34659268/
ΑΙΜΑΤΟΛΟΓΙΚΕΣ ΔΙΑΤΑΡΑΧΕΣ
- Collection of complement-mediated and autoimmune-mediated hematologic conditions after SARS-CoV-2 vaccination: https://ashpublications.org/bloodadvances/article/5/13/2794/476324/Autoimmune-and-complement-mediated-hematologic
Αιμόλυση
- COVID-19 vaccines induce severe hemolysis in paroxysmal nocturnal hemoglobinuria: https://ashpublications.org/blood/article/137/26/3670/475905/COVID-19-vaccines-induce-severe-hemolysis-in
Οξεία λεμφόλυση
- Rituximab-induced acute lympholysis and pancytopenia following vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34429981/
ΝΕΦΡΟΛΟΓΙΚΕΣ ΒΛΑΒΕΣ
Οξεία νεφρική βλάβη
- Minimal change disease with severe acute kidney injury after Oxford-AstraZeneca COVID-19 vaccine: case report: https://pubmed.ncbi.nlm.nih.gov/34242687/.
- Acute kidney injury with macroscopic hematuria and IgA nephropathy after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34352309/
- Minimal change disease and acute kidney injury after Pfizer-BioNTech COVID-19
vaccine: https://pubmed.ncbi.nlm.nih.gov/34000278/
Νεφρωσικό σύνδρομο
- Nephrotic syndrome after ChAdOx1 nCoV-19 vaccine against SARScoV-2: https://pubmed.ncbi.nlm.nih.gov/34250318/.
- New-onset nephrotic syndrome after Janssen COVID-19 vaccination: case report and literature review: https://pubmed.ncbi.nlm.nih.gov/34342187/
Μακροσκοπική αιματουρία
- Hematuria, a generalized petechial rash and headaches after Oxford AstraZeneca ChAdOx1 nCoV-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34620638/
- A case of outbreak of macroscopic hematuria and IgA nephropathy after SARSCoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/33932458/
- Gross hematuria after severe acute respiratory syndrome coronavirus 2 vaccination in 2 patients with IgA nephropathy: https://pubmed.ncbi.nlm.nih.gov/33771584/
ANCA Σπειραματονεφρίτιδα
- ANCA glomerulonephritis following Modern COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34081948/
ΑΝΑΠΑΡΑΓΩΓΙΚΟ ΣΥΣΤΗΜΑ
1). Reis AB, Araújo FC, Pereira VM, Dos Reis AM, Santos RA, Reis FM, 2010. Angiotensin (1–7) and its receptor mas are expressed in the human testis: implications for male infertility. J Mol Histol 41: 75–80. [PubMed] [Google Scholar] DOI: 10.1007/s10735-010-9264-8.
2). Wang Z, Xu X, 2020. ScRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, Leydig and sertoli cells. Cells 9: 920–929.
3). Fu J, Zhou B, Zhang L, Balaji KS, Wei C, Liu X, Chen H, Peng J, Fu J, 2020. Expressions and significances of the angiotensin‐converting enzyme 2 gene, the receptor of SARS‐CoV‐2 for COVID‐19. Mol Biol Rep 47: 4383–4392.
4). Stanley KE, Thomas E, Leaver M, Wells D, 2020. Coronavirus disease (COVID-19) and fertility: viral host entry protein expression in male and female reproductive tissues. Fert Steril 114: 33–43.
5). Shen Q, Xiao X, Aierken A, Liao M, Hua J, 2020. The ACE2 expression in sertoli cells and germ cells may cause male reproductive disorder after SARS-CoV-2 infection. J Cell Mol Med 24: 9472–9477.
6). Vinson GP, Mehta J, Evans S, Matthews S, Puddefoot JR, Saridogan E, Holt WV, Djahanbakhch O, 1996. Angiotensin II stimulates sperm motility. Regul Pept 67: 131–135.
7). Valdivia A, Cortés L, Beitia M, Totorikaguena L, Agirregoitia N, Corcostegui B, Casis L, Matorras R, Irazusta J, Agirregoitia E, 2020. Role of angiotensin-(1–7) via MAS receptor in human sperm motility and acrosome reaction. Reprod 159: 241–249.
8). Aitken RJ, 2020. COVID-19 and human spermatozoa – potential risks for infertility and sexual transmission. Andrology (Epub ahead of print). DOI: 10.1111/andr.12859.
9). Sengupta P, Dutta S, 2020. Does SARS-CoV-2 infection cause sperm DNA fragmentation? Possible link with oxidative stress. Eur J Contracept Reprod Health Care 25: 405–406.
11). Reis FM, Bouissou DR, Pereira VM, Camargos AF, dos Reis AM, Santos RA, 2011. Angiotensin-(1–7), its receptor mas, and the angiotensin-converting enzyme type 2 are expressed in the human ovary. Fertil Steril 95: 176–181.
12). Stanley KE, Thomas E, Leaver M, Wells D, 2020. Coronavirus disease (COVID-19) and fertility: viral host entry protein expression in male and female reproductive tissues. Fert Steril 114: 33–43.
13). Jing Y, Run-Qian L, Hao-Ran W, Hao-Ran C, Ya-Bin L, Yang G, Fei C, 2020. Potential influences of COVID-19/ACE2 on female reproductive system. Mol Hum Reprod 26: 367–373.
14). Chadchan SB, Maurya VK, Popli P, Kommagani R, 2020. The SARS-CoV-2 receptor, angiotensin converting enzyme 2 (ACE2) is required for human endometrial stromal cell decidualization. Biol Reprod (Epub, 2020 Nov 18). Available at: 10.1093/biolre/ioaa211.
15). Jing Y, Run-Qian L, Hao-Ran W, Hao-Ran C, Ya-Bin L, Yang G, et al. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol Hum Reprod. (2020) 26:367–73. doi: 10.1093/molehr/gaaa030.
16). Kotlyar AM, Grechukhina O, Chen A, Popkhadze S, Grimshaw A, Tal O, et al. Vertical transmission of COVID-19: a systematic review and meta-analysis. Am J Obstet Gynecol. (2020) 31:e00087320. doi: 10.1016/j.ajog.2020.07.049.
17). Patanè L, Morotti D, Giunta MR, Sigismondi C, Piccoli MG, Frigerio L, et al. Vertical transmission of coronavirus disease 2019: severe acute respiratory syndrome coronavirus 2 RNA on the fetal side of the placenta in pregnancies with coronavirus disease 2019-positive mothers and neonates at birth. Am J Obstet Gynecol MFM. (2020) 2:100145. doi: 10.1016/j.ajogmf.2020.100145.
18). Baergen RN, Heller DS. Placental pathology in Covid-19 positive mothers: preliminary findings. Pediatr Dev Pathol. (2020) 23:177–80. doi: 10.1177/1093526620925569.
19). C, Dubruc E, Favre G, Greub G, de Leval L, Baud D. SARS-CoV-2 ACE-Receptor detection in the placenta throughout pregnancy. Clin Microbiol Infect. (2020). doi: 10.1016/j.cmi.2020.09.049.
20). Rebecca N Baergen1 and Debra S Heller2 Placental Pathology in Covid-19 Positive Mothers: Preliminary Findings Pediatr Dev Pathol. 2020 Jun; 23(3): 177–180.
21). Ankit Dhaundiyal,a,1 Puja Kumari,b Snehal Sainath Jawalekar,c Gaurav Chauhan,d Sourav Kalra,e,⁎,1 and Umashanker Navikf,⁎⁎,1 Is highly expressed ACE 2 in pregnant women “a curse” in times of COVID-19 pandemic? Life Sci. 2021 Jan 1; 264: 118676.
22). Tom T Shimabukuro 1 , Shin Y Kim 1 , Tanya R Myers 1 , Pedro L Moro 1 , Titilope Oduyebo 1 , Lakshmi Panagiotakopoulos 1 , Paige L Marquez 1 , Christine K Olson 1 , Ruiling Liu 1 , Karen T Chang 1 , Sascha R Ellington 1 , Veronica K Burkel 1 , Ashley N Smoots 1 , Caitlin J Green 1 , Charles Licata 1 , Bicheng C Zhang 1 , Meghna Alimchandani 1 , Adamma Mba-Jonas 1 , Stacey W Martin 1 , Julianne M Gee 1 , Dana M Meaney-Delman 1 , CDC v-safe COVID-19 Pregnancy Registry Team. Preliminary Findings of mRNA Covid-19 Vaccine Safety in Pregnant Persons. N Engl J Med. 2021 Jun 17;384(24):2273-2282. doi: 10.1056.
23). Wang Z, Xu X. ScRNA-seq profiling of human testes reveals the presence of ACE2 receptor, a target for SARS-CoV-2 infection, in spermatogonia, leydig and sertoli cells. Cells. (2020) 9:920. doi: 10.3390/cells9040920.
ΔΕΡΜΑΤΟΛΟΓΙΚΕΣ ΒΛΑΒΕΣ
- Cutaneous adverse effects of available COVID-19 vaccines: https://pubmed.ncbi.nlm.nih.gov/34518015/
- Rare cutaneous adverse effects of COVID-19 vaccines: a case series and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34363637/
- Cutaneous adverse reactions of 35,229 doses of COVID-19 Sinovac and AstraZeneca vaccine COVID-19: a prospective cohort study in health care workers:https://pubmed.ncbi.nlm.nih.gov/34661934/
- A case series of skin reactions to COVID-19 vaccine in the Department of Dermatology at Loma Linda University: https://pubmed.ncbi.nlm.nih.gov/34423106/
- Skin reactions reported after Moderna and Pfizer’s COVID-19 vaccination: a study based on a registry of 414 cases: https://pubmed.ncbi.nlm.nih.gov/33838206/
- Skin reactions after vaccination against SARS-COV-2: a nationwide Spanish crosssectional study of 405 cases: https://pubmed.ncbi.nlm.nih.gov/34254291/
- Late cutaneous reactions after administration of COVID-19 mRNA vaccines: https://www.sciencedirect.com/science/article/pii/S2213219821007996
- Clinical and pathologic correlates of skin reactions to COVID-19 vaccine, including VREPP: a registry-based study: https://www.sciencedirect.com/science/article/pii/S0190962221024427
Πετέχειες
- Petechiae and peeling of fingers after immunization with BTN162b2 messenger RNA (mRNA)-based COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34513435/
- Petechial rash associated with CoronaVac vaccination: first report of cutaneous side effects before phase 3 results: https://ejhp.bmj.com/content/early/2021/05/23/ejhpharm-2021-002794
Ευρυαγγειακή δακτυλιοειδής πορφύρα του Majocchi
- Purpuric rash and thrombocytopenia after mRNA-1273 (Modern) COVID-19 vaccine: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7996471/
- Generalized purpura annularis telangiectodes after SARS-CoV-2 mRNA vaccination: https://pubmed.ncbi.nlm.nih.gov/34236717/
Ψωρίαση
- Onset / outbreak of psoriasis after Corona virus ChAdOx1 nCoV-19 vaccine (Oxford-AstraZeneca / Covishield): report of two cases: https://pubmed.ncbi.nlm.nih.gov/34350668/
- Exacerbation of plaque psoriasis after COVID-19 inactivated mRNA and BNT162b2 vaccines: report of two cases: https://pubmed.ncbi.nlm.nih.gov/34427024/
Πομφολυγώδης φαρμακευτική αντίδραση
- Bullous drug eruption after the second dose of COVID-19 mRNA-1273 (Moderna) vaccine: Case report: https://www.sciencedirect.com/science/article/pii/S1876034121001878.
- Widespread fixed bullous drug eruption after vaccination with ChAdOx1 nCoV-19: https://pubmed.ncbi.nlm.nih.gov/34482558/
Κυστικοπομφολυγώδεις δερματικές αντιδράσεις
- Vesiculobullous cutaneous reactions induced by COVID-19 mRNA vaccine: report of four cases and review of the literature: https://pubmed.ncbi.nlm.nih.gov/34236711/
Νόσος Hailey-Hailey
- Hailey-Hailey disease exacerbation after SARS-CoV-2 vaccination: https://pubmed.ncbi.nlm.nih.gov/34436620/
Ροδόχρους πιτυρίαση
- Case report: Pityriasis rosea-like rash after vaccination with COVID-19: https://pubmed.ncbi.nlm.nih.gov/34557507/
Ουρτικάρια (κνίδωση)
- Increased risk of urticaria/angioedema after BNT162b2 mRNA COVID-19 vaccination in health care workers taking ACE inhibitors: https://pubmed.ncbi.nlm.nih.gov/34579248/
Έλκη Lipschütz (Έλκη αιδοίου)
- Lipschütz ulcers after AstraZeneca COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34366434/.
Τοξική Επιδερμική Νεκρόλυση
- A case of toxic epidermal necrolysis after vaccination with ChAdOx1 nCoV-19 (AZD1222): https://pubmed.ncbi.nlm.nih.gov/34751429/.
Σύνδρομο Sweet
- Sweet’s syndrome after Oxford-AstraZeneca COVID-19 vaccine (AZD1222) in an elderly woman: https://pubmed.ncbi.nlm.nih.gov/34590397/
Αναζωπύρωση VZV – Έρπης Ζωστήρας
- Shingles-like skin lesion after vaccination with AstraZeneca for COVID-19: a case report: https://pubmed.ncbi.nlm.nih.gov/34631069/
- Recurrent herpes zoster after COVID-19 vaccination in patients with chronic urticaria on cyclosporine treatment – A report of 3 cases: https://pubmed.ncbi.nlm.nih.gov/34510694/
- Acute retinal necrosis due to varicella zoster virus reactivation after vaccination with BNT162b2 COVID-19 mRNA: https://pubmed.ncbi.nlm.nih.gov/34851795/.
- Varicella zoster virus and herpes simplex virus reactivation after vaccination with COVID-19: review of 40 cases in an international dermatologic registry: https://pubmed.ncbi.nlm.nih.gov/34487581/
Ηωσινοφιλική Δερμάτωση
1.. Eosinophilic dermatosis after AstraZeneca COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34753210/.
Γυροειδής αλωπεκία
- Recurrence of alopecia areata after covid-19 vaccination: a report of three cases in Italy: https://pubmed.ncbi.nlm.nih.gov/34741583/
ΕΠΙΠΛΟΚΕΣ ΕΓΚΥΜΟΣΥΝΗΣ
- This study notes that 115 pregnant women lost their babies, out of 827 who participated in a study on the safety of covid-19 vaccines: https://www.nejm.org/doi/full/10.1056/NEJMoa2104983.
ΚΑΤΑΣΚΕΥΑΣΤΙΚΕΣ ΑΤΕΛΕΙΕΣ–ΠΡΟΣΜΙΞΕΙΣ
- Process-related impurities in the ChAdOx1 nCov-19 vaccine: https://www.researchsquare.com/article/rs-477964/v1
ΜΥΟΣΚΕΛΕΤΙΚΕΣ ΠΑΡΕΝΕΡΓΕΙΕΣ
- Polyarthralgia and myalgia syndrome after vaccination with ChAdOx1 nCOV-19:https://pubmed.ncbi.nlm.nih.gov/34463066/
- Reactive arthritis after COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34033732/.
Φλεγμονώδης μυοσίτιδα
- Inflammatory myositis after vaccination with ChAdOx1: https://pubmed.ncbi.nlm.nih.gov/34585145/
ΒΛΑΒΕΣ ΕΝΔΟΚΡΙΝΩΝ ΑΔΕΝΩΝ
Θυρεοειδίτιδα
- Three cases of subacute thyroiditis after SARS-CoV-2 vaccination: post-vaccination ASIA syndrome: https://pubmed.ncbi.nlm.nih.gov/34043800/.
Νόσος του Graves
- Two cases of Graves’ disease after SARS-CoV-2 vaccination: an autoimmune /inflammatory syndrome induced by adjuvants: https://pubmed.ncbi.nlm.nih.gov/33858208/
Θυμική υπερπλασία
- Thymic hyperplasia after Covid-19 mRNA-based vaccination with Covid-19: https://pubmed.ncbi.nlm.nih.gov/34462647/
ΠΝΕΥΜΟΝΙΚΕΣ ΒΛΑΒΕΣ
Διάμεση πνευμονίτιδα
- Vaccine-induced interstitial lung disease: a rare reaction to COVID-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34510014/.
Οξεία Ηωσινοφιλική πνευμονία
- Acute eosinophilic pneumonia associated with anti-COVID-19 vaccine AZD1222: https://pubmed.ncbi.nlm.nih.gov/34812326/.
Άσθμα
- Colaneri, M., De Filippo, M., Licari, A., Marseglia, A., Maiocchi, L., Ricciardi, A., Bruno, R. (2021). COVID vaccination and asthma exacerbation: might there be a link? Int J Infect Dis, 112, 243-246. doi:10.1016/j.ijid.2021.09.026. https://www.ncbi.nlm.nih.gov/pubmed/34547487
ΓΕΝΙΚΕΣ ΠΑΘΟΦΥΣΙΟΛΟΓΙΚΕΣ ΒΛΑΒΕΣ
- Extensive investigations revealed consistent pathophysiologic alterations after vaccination with COVID-19 vaccines: https://www.nature.com/articles/s41421-021-00329-3
Διαταραχές βιολογικού μονοπατιού ACE-2
1). M Donoghue 1 , F Hsieh, E Baronas, K Godbout, M Gosselin, N Stagliano, M Donovan, B Woolf, K Robison, R Jeyaseelan, R E Breitbart, S Acton A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9 Circ Res . 2000 Sep 1;87(5):E1-9. DOI: 10.1161/01.res.87.5.e1.
2). S R Tipnis 1 , N M Hooper, R Hyde, E Karran, G Christie, A J Turner A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase 2000 Oct 27;275(43):33238-43. doi: 10.1074/jbc.M002615200. PMID: 10924499.
3). Monika Gooz ADAM-17: The Enzyme That Does It All doi: 10.3109/10409231003628015 PMID: 20184396.
4). Alasdair J. Scott,‡,1 Kieran P. O’Dea,‡,1 David O’Callaghan,‡ Lynn Williams,§ Justina O. Dokpesi,‡ Louise Tatton,‡ Jonathan M. Handy,‡ Philip J. Hogg,¶ and Masao Takata‡,2 Reactive Oxygen Species and p38 Mitogen-activated Protein Kinase Mediate Tumor Necrosis Factor α-Converting Enzyme (TACE/ADAM-17) Activation in Primary Human Monocytes* PMID: 21865167.
5). Pinglong Xu and Rik Derynck Direct activation of TACE-mediated ectodomain shedding by p38 MAP kinase regulates EGF receptor-dependent cell proliferation PMID: 20188673 doi: 10.1016/j.molcel.2010.01.034.
6). M Donoghue 1 , F Hsieh, E Baronas, K Godbout, M Gosselin, N Stagliano, M Donovan, B Woolf, K Robison, R Jeyaseelan, R E Breitbart, S Acton A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9 Circ Res . 2000 Sep 1;87(5):E1-9. DOI: 10.1161/01.res.87.5.e1.
ΣΟΒΑΡΕΣ ΠΑΡΕΝΕΡΓΕΙΕΣ ΣΕ ΥΓΕΙΟΝΟΜΙΚΟΥΣ
- Prevalence of serious adverse events among health care professionals after receiving the first dose of ChAdOx1 nCoV-19 coronavirus vaccine (Covishield) in Togo, March 2021: https://pubmed.ncbi.nlm.nih.gov/34819146/.
ΑΠΟΡΡΙΨΗ ΠΑΓΚΡΕΑΤΙΚΟΥ ΑΛΛΟΜΟΣΧΕΥΜΑΤΟΣ
- Pancreas allograft rejection after ChAdOx1 nCoV-19 vaccine: https://pubmed.ncbi.nlm.nih.gov/34781027/
ΜΕΤΑΒΟΛΙΚΟ ΣΥΝΔΡΟΜΟ
- Change in blood viscosity after COVID-19 vaccination: estimation for persons with underlying metabolic syndrome: https://pubmed.ncbi.nlm.nih.gov/34868465/
ΝΕΟΠΛΑΣΙΕΣ
Αγγειοανοσοβλαστικό Τ–κυτταρικό λέμφωμα
- Rapid progression of angioimmunoblastic T-cell lymphoma after BNT162b2 mRNA booster vaccination: case report: https://www.frontiersin.org/articles/10.3389/fmed.2021.798095/
Καρκίνος πνεύμονα εκ πλακωδών επιθηλιακών κυττάρων
- Squamous cell carcinoma of the lung with hemoptysis following vaccination with
tozinameran (BNT162b2, Pfizer-BioNTech): https://pubmed.ncbi.nlm.nih.gov/
34612003/
ΕΓΚΕΦΑΛΙΚΟΣ ΘΑΝΑΤΟΣ
- Brain death in a vaccinated patient with COVID-19 infection: https://pubmed.ncbi.nlm.nih.gov/34656887/
ΓΑΣΤΡΟΠΑΡΕΣΗ
- Gastroparesis after Pfizer-BioNTech COVID-19 vaccination: https://pubmed.ncbi.nlm.nih.gov/34187985/
ΑΣΦΑΛΕΙΑ ΣΤΗΝ ΕΦΗΒΕΙΑ
- Dimopoulou, D., Spyridis, N., Vartzelis, G., Tsolia, M. N., & Maritsi, D. N. (2021). Safety and tolerability of the COVID-19 mRNA-vaccine in adolescents with juvenile idiopathic arthritis on treatment with TNF-inhibitors. Arthritis Rheumatol. doi:10.1002/art.41977. https://www.ncbi.nlm.nih.gov/pubmed/34492161
- Hause, A. M., Gee, J., Baggs, J., Abara, W. E., Marquez, P., Thompson, D., . . . Shay, D. K. (2021). COVID-19 Vaccine Safety in Adolescents Aged 12-17 Years – United States, December 14, 2020-July 16, 2021. MMWR Morb Mortal Wkly Rep, 70(31),1053-1058. doi:10.15585/mmwr.mm7031e1. https://www.ncbi.nlm.nih.gov/pubmed/34351881
Δεν υπάρχουν σχόλια:
Δημοσίευση σχολίου